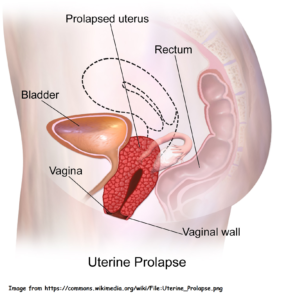
 This refers to the descend of the uterus into the lower half of the vagina and beyond. In its most severe form, the whole uterus may be outside the vagina. Besides the uterus, other pelvic organ may descend as well such as bladder (cystocoele), rectum (rectocoele) and the small intestines (enterocoele).
This refers to the descend of the uterus into the lower half of the vagina and beyond. In its most severe form, the whole uterus may be outside the vagina. Besides the uterus, other pelvic organ may descend as well such as bladder (cystocoele), rectum (rectocoele) and the small intestines (enterocoele).
Symptoms and signs
- A lump is seen or felt at the opening of the vagina. It may be seen protruding outside of the vagina.
- Vague discomfort or pressure in the pelvic region.
- Backache that worsens with lifting.

- Urination problems such as frequent and painful urination, difficulty in urination. occasional stress incontinence (urine leakage when laughing, sneezing or coughing), inability to control urination (uncontrollable urine leakage).
- Difficulty in defecation.
- Pain during or difficulty with sexual intercourse.
- Abnormal per vaginal bleeding, usually arising from the exposed vagina wall and cervix.
Causes
Prolapse occurs when muscles and ligaments at the base of the abdomen (pelvic floor) become extremely stretched and weakened.
Risk factors
- Repeated childbirth, although one pregnancy and vaginal delivery can weaken the area enough to lead to eventual prolapse.

- Difficult vaginal delivery – trauma and lacerations sustained during labor and delivery, difficult forceps delivery, delivery of a big baby.
- Advancing age; decreased oestrogen (e.g., menopause).
- Conditions that cause increased intra-abdominal pressure such as abdominal tumours, chronic coughing, chronic constipation.
- Obesity.
- Occupations requiring heavy lifting.
Prevention
- Maintain appropriate weight.
- Practice pelvic-strengthening exercises during pregnancy and after childbirth.
- Eat a normal, well-balanced diet.
- Engage in a regular exercise program to maintain good muscle strength.
- Avoid constipation.
Expected outcome
Many women are able to cope with mild prolapse and surgery is not always necessary. The uterine prolapse itself does not pose a significant health risk.
Possible complications
- Ulceration of the cervix and vagina walls.
- Increased risk of bladder infection.
- Urinary tract obstruction.
- Constipation, leading to haemorrhoids.
Treatment
- Clinical examinations include pelvic examination, Thin Prep (Pap smear), urinalysis and pelvic ultrasound sound scan. Am ultrasound scan of the abdomen may be done to look at the kidneys and excluded any intra-abdominal masses that can predispose to uterine prolapse.
- A treatment plan depends on severity of prolapse, age, associated symptoms, sexual activity, associated pelvic disorders, and desire for future pregnancy.
- Patients with mild symptoms can usually be treated initially with an exercise program (Kegel). Kegel exercise is a form of training to recognize, control and strengthen the pelvic muscles. These are the ones you use to interrupt urination in mid-stream.
- Avoid wearing tight girdles or clothing that increases intra-abdominal pressure.
- Avoid occupational or physical activities that increase intra-abdominal pressure.
- You should reduce weight if you are overweight.
- Eat a diet high in fiber to prevent constipation.

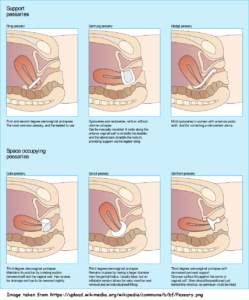
- A pessary (small device that is inserted into the vagina to help maintain the uterus in a normal position) may recommended. Most pessaries are made from medical grade silicone and come in different shapes, sizes and are individually fitted. It’s important to get the right fit. The pessary may fall out if it is too small. If it is too big, it may cause pain, bleeding or difficulty in urination or passing motion. If these happen, you should see your doctor as soon as possible for removal or refitting a more appropriate size pessary. Your doctor will advise a follow-up schedule to check the pessary, or remove for cleaning, or change to a new one. Not all women will find the pessary helpful but it is worth a try if you are not keen for surgery. You should discuss this option with your doctor.

- Surgical measures may be necessary when the prolapse causes significant symptoms. Several methods are available and the choice will depend on a number of variables and the presence of associated conditions. One of the most commonly recommended surgery is the vaginal hysterectomy (removal of the uterus and cervix) pelvic floor repair. Pelvic floor repair is an operation carried out to correct the vaginal wall prolapse. It will help to push the bladder and rectum back to its normal position and strengthen the vaginal wall at the same time via sutures (which are disposables). However, a small number of women may experience recurrence of prolapse later in life. Therefore, you should be aware of all the predisposing factors for prolapse and act accordingly to avoid them.
To print a pdf copy, click HERE
[mailerlite_form form_id=3]