The main purpose of contraception (or birth control) is to prevent an unplanned pregnancy. Most methods of contraception enable sexually active couples to temporarily avoid pregnancy. Emergency contraception (or post-coital contraception) is used in preventing pregnancy after intercourse when standard contraceptives have failed, when no contraceptives were used at all or in cases of sexual assault. Emergency contraception is not considered an abortion. However, it is not recommended to be used as regular contraception. Emergency contraception is generally effective for birth control (75-90%), but effectiveness varies depending on the time of the woman’s menstrual cycle and the timing of the prior sexual activity.
Mechanism of actions – a single mechanism has not been established. EC methods are not abortifacient. Possible mechanisms are:
– Prevent or postpone ovulation.
– Causing genital tract to be hostile to sperm or blastocyst.
– Interferes with tubal transport.
– Preventing fertilisation (with IUD use).
– Blocking implantation (with IUD use).
Type of emergency contraception
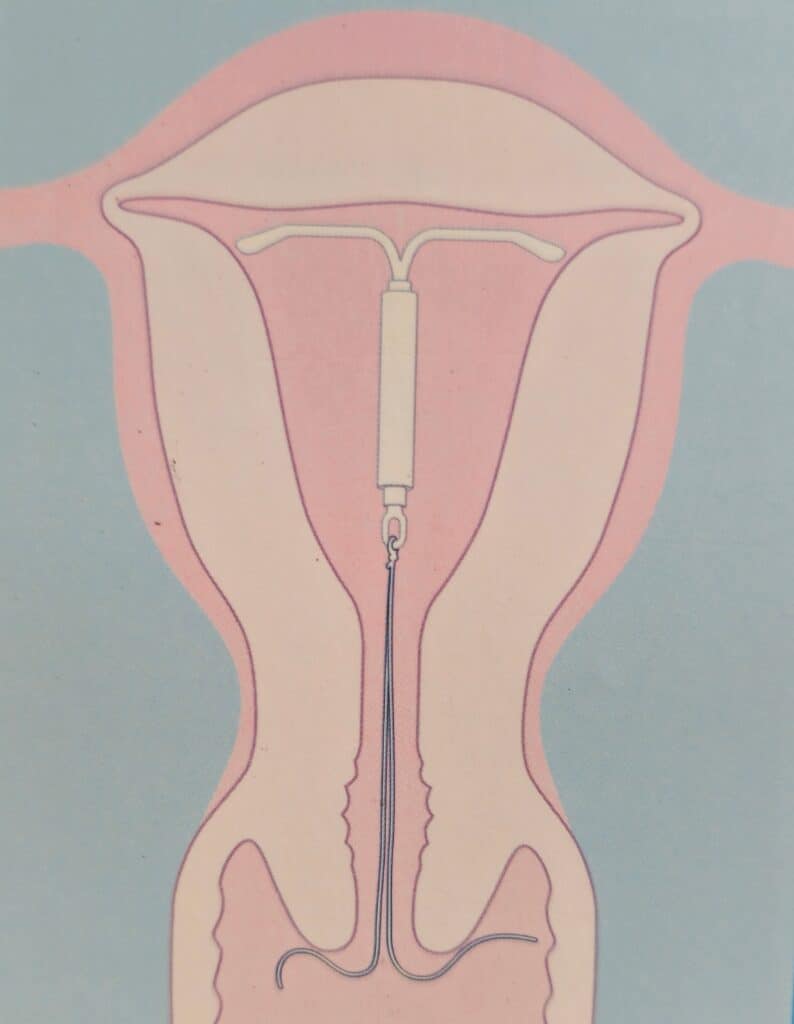
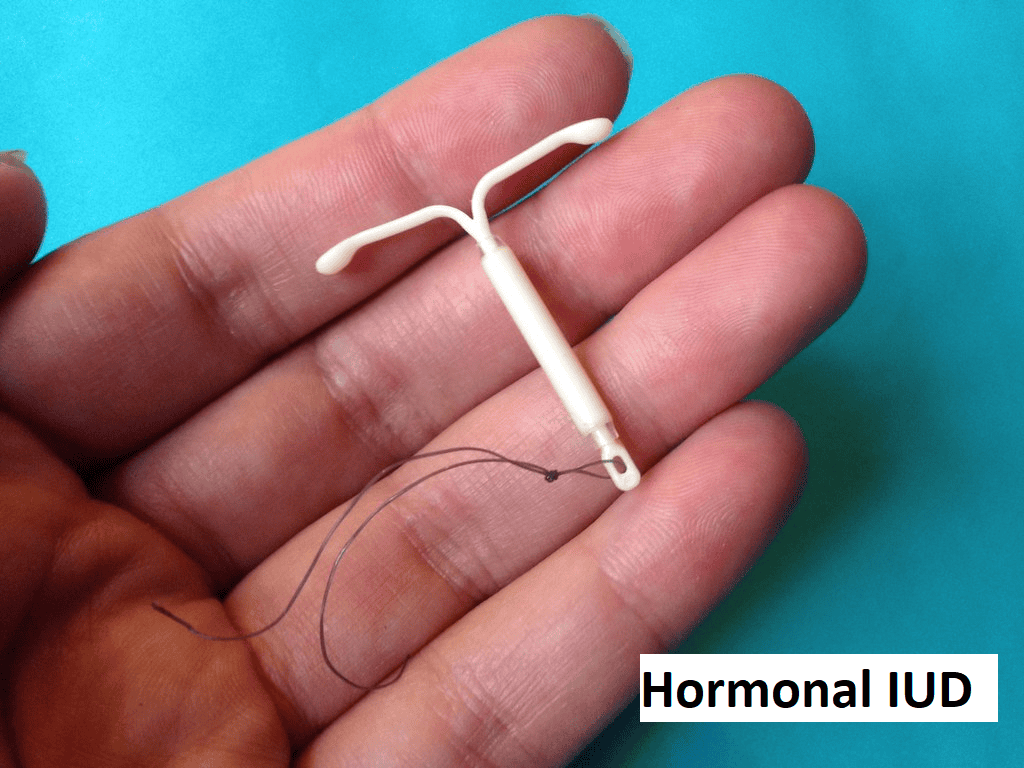
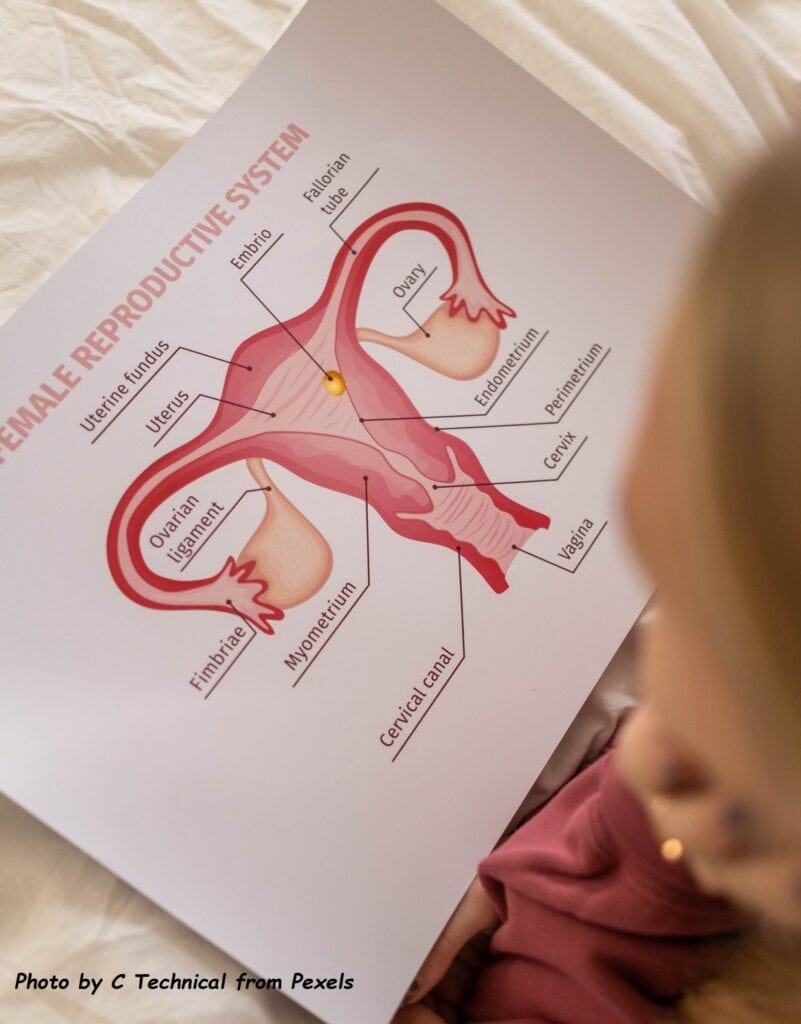
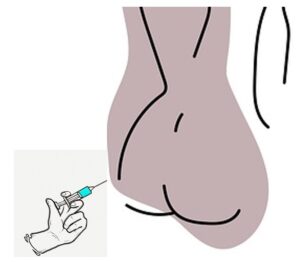
1. Intrauterine Contraceptive Device (IUD or IUCD) – An IUD is a birth control device that is inserted into a woman’s uterus by a doctor
Insertion of copper IUD should not be more than five days after unprotected intercourse. This is suitable for those who desire long-term contraception. The placement has risks of pelvic infection and uterine injury, although these are quite rare. In a small group of women, long-term use of an IUD for birth control may cause certain side effects, such as heavy menstrual bleeding and painful menstrual cramps. It can be removed easily in the clinic if unsuitable.
This is the only method of EC that is effective after ovulation has taken place, therefore, making it the most effective method among all the emergency contraceptive choices and ideal for those who want long-term contraception.

2. Hormones pills:
A. Progesterone receptor modulator – the drug is ulipristal acetate, marketed as ella®.

It is given as 30 mg single oral dose, within 5 days (120 hours) after unprotected intercourse or contraceptive failure. This should be the hormonal emergency contraception of choice in view of the higher effectiveness and fewer side effects when compared to the levonorgestrel or combined hormonal contraception.
B. Progestogen-only emergency contraception – the hormone used is levonorgestrel. The dosage is 1.5 gm as a single dose. This is better than the divided dose of 0.75mg given 12 hours apart. Ideally, it should be taken within 72 hours of unprotected intercourse. Commercial brand available are Madonna, Postinor-2, Escapelle.

C. Combined hormonal contraception (Yuzpe regime) – each dose should consist of ethinyl oestradiol (EE) 100 mcg and levonorgestrel (LNG) 500 mcg. Two doses are required. There are no commercial brands available for this regimen. However, this can be made from a variety of available combined oral contraceptives pills in the market. The dosage sgould be taken within 72 hours of unprotected intercourse and repeat another dose in 12 hours. This is the least effective among the oral pills.
The most effective EC method is the intrauterine device (IUD). The risk of pregnancy following placement of a copper IUD is 0.1%. For oral types, the most effective is ulipristal acetate, followed by the levonorgestrel. Data from trials comparing ulipristal acetate and levonorgestrel report respective pregnancy rates of 1.8% for ulipristal acetate versus 2.6% for levonorgestrel. However, it is important to take note that these are ideal situations and the failure rate is higher if oral EC is taken after ovulation or the longer the interval between having unprotected intercourse and taking the EC. Higher body weight or BMI could also reduce the effectiveness of oral EC, particularly the levonorgestrel and Yutze regime.
Oral EC pills can be used more than once in a cycle. Repeated doses may result in more irregular bleeding and side effects. You should discuss this with your healthcare provider if you are planning to use this more than once in one cycle. In terms of contraindication, ulipristal should be avoided in women with severe asthma on oral steroids. Other than this, it is generally safe to use ulipristal and levonorgestrel in the majority of healthy women.
Disadvantages of Emergency Contraception
- Not as effective as other forms of regular birth controls.
- Side effects include nausea, vomiting, headache, breast tenderness, bloated feeling and swelling of hands and feet. The side effects may be less with the ulipristal or levonorgestrel and more severe with the use of the combined oestrogen and progestogen formulation (Yutzpe regime).
- Further contraception is required
- Certain medications taken before or after the use of oral emergency contraception may reduce the efficacy – please discuss with your doctor regarding these drug interactions.
Following the use of EC, you should:

- Use a barrier method until the next period.
- If vomiting occurs within 3 hours of taking oral EC, a repeat dose should be given.
- Talk to your health care provider regarding long-term contraception choices.
- Seek medical advice if you experience unexpected side effects. Or if menses is delayed by more than seven days, or has abnormal flow, and you suspect that you may be pregnant.
Menses following administration of EC pills:
- 75 to 90% menstruate within seven days (before or after) of their expected date of the next menses.
- Menstrual bleeding will be late in the remaining 10 to 20%.
Disclaimer
This is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. It is important for readers to seek proper medical advice when necessary.