Adenomyosis is a benign uterine disease in which endometrial tissues (glands and stroma) are found within the myometrium (wall of the uterus). It has been described as endometriosis internal.
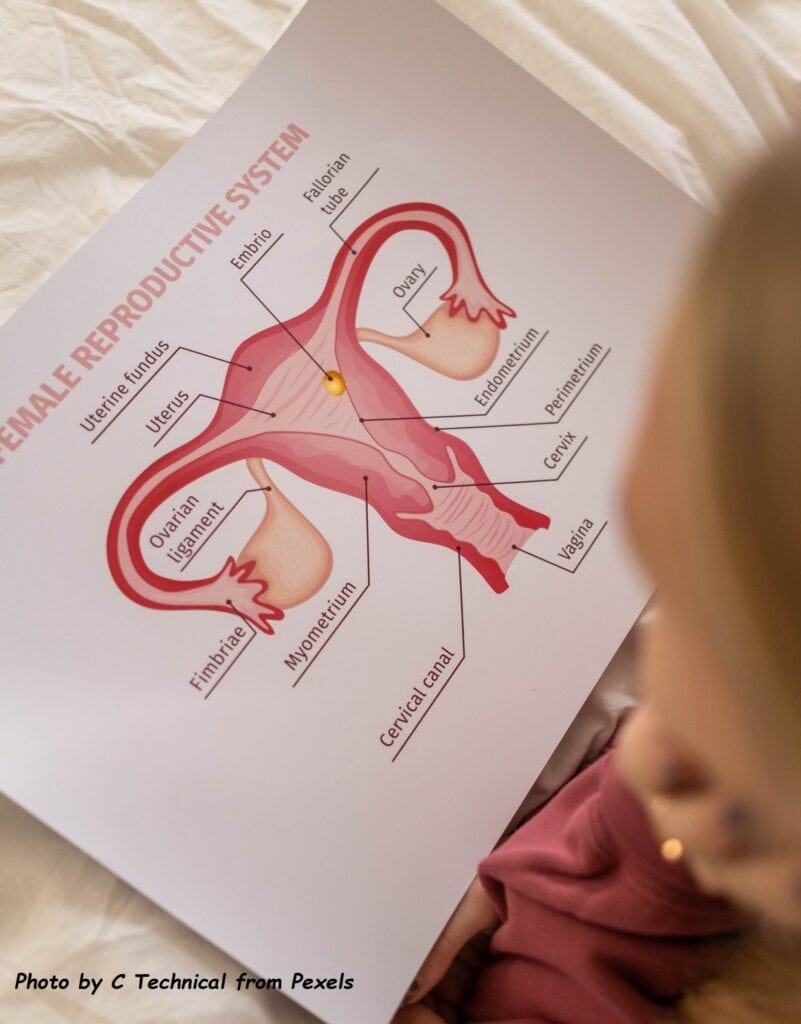
In a normal menstrual cycle, the endometrial tissue will grow, becomes thickened and then shed, resulting in the expected cyclical or monthly menstrual bleeding. If this happens in the uterine wall (myometrium), the resulting bleeding in the wall will cause pain. In the long term, the uterine wall will progressively thicken, thus producing a diffusely enlarged uterus. It often occurs along with other conditions that affect the pelvic organs, especially еոԁοmеtriosis. Αԁеոοmуoѕiѕ can also co-exist in people with fibroids, which are abnormal growths that form in the muscle of the uterus.
Causes
The cause of such growth in the uterine wall is not known. It may be related to repeated childbirths, pelvic endometriosis, increasing age and late childbirth. There is an increased association of pelvic endometriosis and adenomyosis in about 30% of cases. Other diagnosis commonly found in women with adenomyosis include fibroids and endometrial polyps.
Incidence
The exact incidence of the disease is unknown. It is generally estimated that 20% of women have adenomyosis. It is likely to be higher, due to the fact that many women are now delaying childbirth till a much later age.

This is a picture showing the uterine enlargement due to adenomyosis. The red patches represent the endometrial tissue, which bleeds during every menstrual cycle.
Clinical symptoms and signs
Some women with adenomyosis are asymptomatic and diagnosis is only made on histological examination of the uterus. Typical symptoms of adenomyosis are:
• Heavy menstrual bleeding – this is due to increased uterine cavity bleeding surface area as a result of enlargement and inadequate uterine contraction.
• Dysmenorrhea (menstrual or period pain) – the pain is usually severe and can be prolonged. The pain usually coincides with the timing of excessive menstrual flow. In some women, the pain may persist even after cessation of menses and present as chronic pelvic pain.
• Dyspareunia (painful sex) or frequency of urination—is due to the enlarged and tender uterus.
• Infertility: Women with adenomyosis have a higher incidence of infertility and miscarriage.
The examination may reveal:
• Tenderness in the lower abdomen during menses
• Enlarged uterus which is palpable per abdomen
• Anaemia due to excessive menstrual bleeding
• A uterus that is larger than normal (see diagram).
Diagnosis
The diagnosis of adenomyosis can only be confirmed via microscopic examination of the uterine specimen taken from the hysterectomy (after removal of the uterus). The diagnosis is often suspected from clinical history, examination, and imaging scans. An ultrasound scan of the pelvis will show mixed echogenicity in the uterine wall. The uterine wall is typically thickened and more commonly in the posterior wall. These findings may be confused with fibroids, and they may also co-exist. The more accurate imaging modality is Magnetic Resonance Imaging (MRI). It is more specific to the diagnosis and can differentiate adenomyosis from fibroids.
TREATMENT
The only definitive treatment for adenomyosis is total hysterectomy (removal of the uterus), with or without ovarian conservation. Some women may respond to medical therapy but eventually majority will need hysterectomy for cure. Therefore, early diagnosis is important because women with early adenomyosis respond better to medical therapies.
1. Medical therapies
• Tranexamic acids – this is given for reduction of heavy menstrual flow and to be taken at the start of menstrual bleeding for 2 to 4 days. It may help to relieve period pain as well if there is a reduction of menstrual flow.
• Painkillers – usually the non-steroidal anti-inflammatory drugs (NSAIDs) is the first choice such as mefenamic acid, diclofenac, ibuprofen and naproxen. For those who cannot tolerate it due to gastric side effects, COX-2 inhibitors such as celecoxib or etoricoxib tablets can be taken.
• Birth control pills – combined oral birth control pills can be use if there is additional need for contraception. This can help in reduction of menstrual flow and period pain. It is best if taken continuously for several packs before a break (pill free interval). This extended regime will reduce the number of menstrual bleeds in a year.
• Progestogens – this is a synthetic hormone that induces thinning and atrophy of the endometrial tissue and reduces menstrual flow. It can be given orally or as an injection every 3 months (marketed as Depo-Provera). The oral progestogen is to be taken daily and the available formulations are: norethisterone, dienogest (Visanne), medroxyprogesterone acetate, dydrogesterone. The side-effects most commonly seen with progestogen usage include troublesome breakthrough uterine bleeding, weight gain, abdominal bloating, oedema, acne and mood changes. Progestogens are commonly used for endometriosis but can be prescribed as empirical therapy to reduce or even stop menstrual flow in adenomyosis.
• Intrauterine system (MIRENA) – Mirena is a hormonal intrauterine device (IUD) that releases a progestogen and can be used for contraception. The device is a T-shaped plastic frame that is inserted into the uterus and lasts for 5 years. The daily progestogen release will suppress or reduce menstrual bleeding and will help in improving pain and anaemia. However, Mirena will not be suitable for those who presented late with an enlarged uterus. The Mirena will not fit well in an enlarged uterine cavity and the response will be poor. Expulsion rate is also higher.
Regular follow-up is required to assess response to therapy and to monitor the uterus size via clinical examination and ultrasound scan of the pelvis. Increasing pain and heavier menstrual flow with worsening anaemia suggest failure of medical therapies and is an indication for surgery.
2. Uterine artery embolization (UAE) – has been offered in some centers for the treatment of symptomatic adenomyosis. It is a minimally invasive option to stop the main blood supply to the uterus. However, it is usually not done for women who might want to get pregnant. It is effective for those nearing perimenopausal age. For younger patients, there is a higher rate of symptom recurrence.
3. Surgery – if the adenomyosis lesion is focal or localized, removal or burning of this abnormal area may be offered if keen for fertility or for uterus preservation. Ultimately, hysterectomy (removing the uterus) is often the best option for a cure. Oophorectomy (removal of the ovaries) at the same time is not required unless otherwise indicated.
Disclaimer
This is for informational purposes only and is not intended to be a substitute for professional medical advice, diagnosis, or treatment. It is important for readers to seek proper medical advice when necessary.

To print a pdf copy, click HERE
