Heavy menstrual bleeding or HMB (previously called menorrhagia) is a significant cause of morbidity in women of reproductive age. It often involves soaking through ten or more sanitary napkins in a day, a menstrual flow that lasts for seven to 14 days or even longer. The presence of “flooding” or clots is indicative of heavy bleeding. Normal menstrual blood flows freely without clotting. This is because of the presence of an anti-clotting agent produced by the uterus. However, if the bleeding is excessive and far exceeds the amount of anti-clotting agent available, then the remaining blood that flows out will form clots. Bleeding between menstrual cycles is also abnormal. The presence of other clinical signs such as anaemia will further support the diagnosis and indicate the severity of the bleeding
Heavy menstrual bleeding or HMB (previously called menorrhagia) is a significant cause of morbidity in women of reproductive age. It often involves soaking through ten or more sanitary napkins in a day, a menstrual flow that lasts for seven to 14 days or even longer. The presence of “flooding” or clots is indicative of heavy bleeding. Normal menstrual blood flows freely without clotting. This is because of the presence of an anti-clotting agent produced by the uterus. However, if the bleeding is excessive and far exceeds the amount of anti-clotting agent available, then the remaining blood that flows out will form clots. Bleeding between menstrual cycles is also abnormal. The presence of other clinical signs such as anaemia will further support the diagnosis and indicate the severity of the bleeding
 Several community prevalence studies found that approximately 30% of women of reproductive age had complained of heavy periods at any one time. In the United Kingdom, referrals for menstrual disorders account for about 20% of all referrals to specialist gynaecology services, placing a significant burden on healthcare services. It is therefore common and can affect the quality of life for many women. Women with HMB may have difficulties coping with work and social activities. They often have psychological problems such as anxiety and depression and their sex lives may also be affected. Fear of bleeding further prevents some of these women from traveling. The presence of anaemia will further worsen the quality of life.
Several community prevalence studies found that approximately 30% of women of reproductive age had complained of heavy periods at any one time. In the United Kingdom, referrals for menstrual disorders account for about 20% of all referrals to specialist gynaecology services, placing a significant burden on healthcare services. It is therefore common and can affect the quality of life for many women. Women with HMB may have difficulties coping with work and social activities. They often have psychological problems such as anxiety and depression and their sex lives may also be affected. Fear of bleeding further prevents some of these women from traveling. The presence of anaemia will further worsen the quality of life.
Causes of HMB:
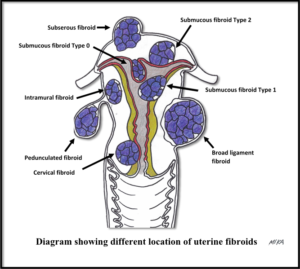
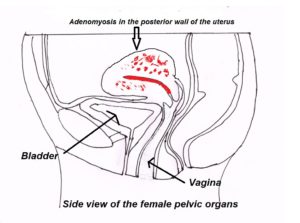
- Growths in the uterus such as fibroids, adenomyosis, endometrial polyps, and cancerous lesions (either uterus or cervix).
- Abnormal ovulatory cycles and the local endometrial factors (the area which shed during menses). This is often found in approximately 50% of cases of HMB. Often, there is an overgrowth of the endometrium (inner lining of the uterus) due to hormonal imbalance.
- Medical diseases such as clotting disorders.
- Due to certain medications that may alter the coagulation pathway, hormones therapy and use of the intrauterine device.
The risk of HMB increases with polycystic ovary syndrome (PCOS), obesity, and age.
Possible complications:
- Anemia from heavy bleeding may require a blood transfusion.
- Cancer (higher risk if the disorder is untreated).
- Infertility resulting from lack of ovulation (release of the egg from the ovary).
Investigations
 The primary goal of the clinical evaluation of HMB is to establish a specific diagnosis and to rule out either cervical cancer, endometrial cancer, and endometrial hyperplasia. A general physical examination will be done to exclude other medical conditions that may cause HMB, followed by a pelvic examination and ultrasound scan. A Pap smear (Cervical cytology) screening is advised if clinically indicated and is done when there is no or minimal bleeding. A blood test may be necessary, especially to evaluate your haemoglobin level. Endometrial biopsy is considered if the woman is above the age of 40 or if there is anything in the history to suggest the need to exclude endometrial cancer or hyperplasia. In some cases, a diagnostic hysteroscopy is required when an intrauterine pathology (such as endometrial polyps or fibroids) is suspected from the ultrasound scan. Up to this stage, a diagnosis will be made in most if not all cases of HMB.
The primary goal of the clinical evaluation of HMB is to establish a specific diagnosis and to rule out either cervical cancer, endometrial cancer, and endometrial hyperplasia. A general physical examination will be done to exclude other medical conditions that may cause HMB, followed by a pelvic examination and ultrasound scan. A Pap smear (Cervical cytology) screening is advised if clinically indicated and is done when there is no or minimal bleeding. A blood test may be necessary, especially to evaluate your haemoglobin level. Endometrial biopsy is considered if the woman is above the age of 40 or if there is anything in the history to suggest the need to exclude endometrial cancer or hyperplasia. In some cases, a diagnostic hysteroscopy is required when an intrauterine pathology (such as endometrial polyps or fibroids) is suspected from the ultrasound scan. Up to this stage, a diagnosis will be made in most if not all cases of HMB.
Treatment
Treatment is directed to stopping the excessive bleeding, correcting the anemia (either with blood transfusion or intravenous infusion of iron) and to follow up response to the therapy. If bleeding is severe, hospitalization may be necessary to bring it under control.
Oral Iron supplements will be given for mild anemia. Treatment is directed towards the specific cause. The options for treating HMB include:
 A. Medical
A. Medical
Taking medicine to reduce bleeding. This is usually the first-line therapy, and the most commonly used drugs are tranexamic acid (an antifibrinolytic drug), non-steroidal anti-inflammatory drugs (NSAIDs, such as diclofenac, mefenamic acid, naproxen), and hormonal pills such as progestogen. Many contraceptives (family planning) methods can also help to reduce the significant amount of menstrual flow and are often advocated for long-term control. Some of these methods may even give rise to absent or minimal menses while you are taking them. Discuss these with your doctor to choose the best method to suit your needs. It can either be taken orally (including the combined oral contraceptive or progestogen-only pills), as injectables, as implant or an intrauterine device. The intrauterine device (levonorgestrel-releasing intrauterine system – MIRENA) is placed inside the uterine cavity and releases a small amount of hormone daily to slow down the growth of the endometrium. It can reduce the menstrual flow significantly and, in some women, they may not have menses at all. It can last for 5 years and is suitable for long-term treatment of HMB.
B. Surgery
- If intrauterine pathology such as sub-mucous fibroids or endometrial polyps is found during the investigation, these can be removed with the hysteroscope and can be done as a daycare procedure (hysteroscopic surgery).
- The presence of fibroids may require surgical removal (myomectomy). Some cases of HMB due to fibroid or adenomyosis may be suitable for uterine artery embolization (UAE) or High-intensity focused ultrasound (HIFU).
- Endometrial ablation – in this surgery, the endometrium layers are removed, either through the hysteroscope or destroyed using the newer ablative devices, whilst leaving the uterus intact. It is done as a daycare procedure. However, not all women are suitable for this type of treatment.
- Hysterectomy (having the uterus removed). This is often the last resort, when medical therapy fails to relieve the bleeding or when there is the presence of other co-existing pathologies such as large fibroids, endometriosis, ovarian cysts, or cancerous lesions.
 Although medical therapy is the first-line treatment for benign causes of HMB, it is not universally effective. In some patients, it can give rise to undesirable side effects. In such instances when there is failed medical therapy, surgery (including non-invasive options) is the next alternative. Therefore, the appropriate choice should be made jointly by the woman and the clinician responsible for the treatment. This decision should be based on the underlying clinical condition, anatomical suitability, the desired outcome of the treatment (whether the woman is happy with reduced menstrual bleeding or insist on complete cessation of menstrual bleeding), completion of family, the relative benefits of all other treatment options and the adverse events associated with them.
Although medical therapy is the first-line treatment for benign causes of HMB, it is not universally effective. In some patients, it can give rise to undesirable side effects. In such instances when there is failed medical therapy, surgery (including non-invasive options) is the next alternative. Therefore, the appropriate choice should be made jointly by the woman and the clinician responsible for the treatment. This decision should be based on the underlying clinical condition, anatomical suitability, the desired outcome of the treatment (whether the woman is happy with reduced menstrual bleeding or insist on complete cessation of menstrual bleeding), completion of family, the relative benefits of all other treatment options and the adverse events associated with them.
You should see your doctor immediately if this occurs during or after treatment:
- Bleeding becomes excessive (soaking a pad or tampon more often than once every 1 to 2 hours).
- Feeling unwell, headache, dizziness, fever, or muscle aches.
- New, unexplained symptoms develop. Drugs used in treatment may produce some side effects.
To print a pdf copy, click HERE
[mailerlite_form form_id=3]