 Treatment for infertility will depend on the underlying cause. Unfortunately, not all causes can be treated by surgery, medications, or both. Even if the suspected underlying cause of infertility has been treated, not all women will conceive. In about 10% to 15% of infertile couples, the cause is usually not found after a standard clinical and laboratory evaluation. This is term as unexplained infertility. Deciding what to do, if anything, when a fertility evaluation is completed may not be easy. Any treatment for conceiving is actually “maximizing fertility potential” rather than “curing infertility.” There is no guarantee that any of them will result in the successful birth of a baby. Ultimately, if conventional therapies do not achieve the desired pregnancy, then the last resort will be assisted reproductive technology (ART). This refers to procedures such as in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI).
Treatment for infertility will depend on the underlying cause. Unfortunately, not all causes can be treated by surgery, medications, or both. Even if the suspected underlying cause of infertility has been treated, not all women will conceive. In about 10% to 15% of infertile couples, the cause is usually not found after a standard clinical and laboratory evaluation. This is term as unexplained infertility. Deciding what to do, if anything, when a fertility evaluation is completed may not be easy. Any treatment for conceiving is actually “maximizing fertility potential” rather than “curing infertility.” There is no guarantee that any of them will result in the successful birth of a baby. Ultimately, if conventional therapies do not achieve the desired pregnancy, then the last resort will be assisted reproductive technology (ART). This refers to procedures such as in vitro fertilization (IVF) and intracytoplasmic sperm injection (ICSI).
The cost of infertility treatment can be very high and generally not covered by insurance. The process of initial evaluation and subsequent treatment may involve many procedures and visits to the doctor. Therefore, it can be a stressful period and a test of the couple’s patience.
Ovulation induction drugs
Fertility drugs can be either in oral or injection forms. Oral ovulation induction drugs include clomiphene citrate or letrozole, which is usually given to women who are not ovulating regularly. It may also be given primarily to increase the number of eggs, hoping to improve the fertilization chance. Couples are then advised either to do timed sex (at the time of ovulation) or undergo intrauterine insemination. Other ovulation induction drugs in injection forms that are commonly used include human menopausal gonadotropin (hMG) and follicular stimulating hormone (FSH). These drugs are expensive and therefore, it is only used in combination with intrauterine insemination or ART procedures.
Side effects of these drugs are multiple pregnancies, excessive stimulation resulting in abdominal distention, ovary enlargement and pain (Ovarian Hyperstimulation Syndrome or OHSS).
Surgery in the male
 Some men may have a varicocele, which is a collection of swollen veins in the scrotum that often looks and feels like a bag of worms but may be less obvious. Some men with a varicocele are fertile. For those who seemingly are not and whose sperm are sluggish, surgical repair of the varicocele may improve their chances of fatherhood. However, there is some debate about when the operation is appropriate. It may not be recommended unless other reasons for the infertility are not found.
Some men may have a varicocele, which is a collection of swollen veins in the scrotum that often looks and feels like a bag of worms but may be less obvious. Some men with a varicocele are fertile. For those who seemingly are not and whose sperm are sluggish, surgical repair of the varicocele may improve their chances of fatherhood. However, there is some debate about when the operation is appropriate. It may not be recommended unless other reasons for the infertility are not found.
Another male infertility problem can be due to the damage of the vas deferens resulting in blockage. The vas deferens is the passage through which sperm must pass for ejaculation. The blockage can be due to vasectomy (male sterilization), scar tissue formation caused by earlier unrelated surgery, a sexually transmitted disease or other infections. Reversal of blockage can be done but the results are often disappointing. Alternatively, sperm aspiration through the vas deferens or directly into the testes can be attempted. If healthy and motile sperms are present, these can be used for ART procedures (see below).
Surgery in the female
This may include:
1. Tubal surgery (repair or reversal of blockage) – this is indicated in women with a proven tubal blockage that is amenable to surgery such as a previous sterilization procedure called tubal ligation, damage to the tubes by earlier unrelated surgery or infection. However, successful surgical repairs of damaged fallopian tubes do not necessarily mean that any eggs fertilized in them will be able to make their way to the uterus. Sometimes, an ectopic pregnancy occurs, in which the fertilized egg gets trapped in the tube where it cannot survive when it grows. Any woman can have an ectopic pregnancy, but those whose tubes have been damaged are at the greatest risk, even after corrective surgery. Tubal repair now is uncommon due to the higher success rate with ART procedures.
2. Repair of uterine abnormalities such as uterine cavity adhesions (Ashermann Syndrome) or structural abnormalities (such as uterine septum)
3. Myomectomy (fibroids removal) – the only type of fibroids that has been associated with reduced fertility is the submucous variety (fibroids protruding into the uterine cavity). The procedure of choice to remove this type of fibroids is with the use of the operative hysteroscope (hysteroscopic myomectomy). In a hysteroscopic myomectomy, a telescopic instrument (hysteroscope) and small surgical instruments are inserted into the uterus through the vagina and cervix to cut and remove the fibroids. This instrument has a built-in wire loop and uses an electrical current to cut out the fibroids. In this method, there is no surgical incision or skin scarring. Postoperative recovery is also quicker, with no or very minimal pain.
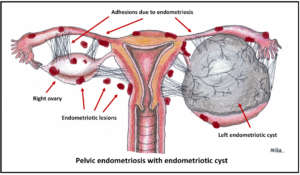 4. Endometriosis can cause or contribute to infertility when small pieces of the uterine lining escape and take up residence on the surfaces of organs in the abdominal cavity. Inflammation and regular monthly bleeding will eventually lead to chronic irritation and significant internal scarring of the ovaries, fallopian tubes, inner or outer walls of the uterus, or other nearby structures. This damages the pelvic organs, thus resulting in infertility. Both surgery and drug treatments (sometimes combined) are used to treat endometriosis.
4. Endometriosis can cause or contribute to infertility when small pieces of the uterine lining escape and take up residence on the surfaces of organs in the abdominal cavity. Inflammation and regular monthly bleeding will eventually lead to chronic irritation and significant internal scarring of the ovaries, fallopian tubes, inner or outer walls of the uterus, or other nearby structures. This damages the pelvic organs, thus resulting in infertility. Both surgery and drug treatments (sometimes combined) are used to treat endometriosis.
Intrauterine insemination (IUI)
Intrauterine insemination (IUI) refers to a procedure whereby the washed semen is placed into the uterine cavity using a hollow, flexible catheter (small tube). Criteria to be eligible for IUI will include at least one patent fallopian tube and adequate sperm quality. This is done in the doctor’s office. All inseminations are performed around the time the woman should be ovulating, either naturally or after using a fertility drug. The semen may be from the woman’s husband or from a donor.
Sperm washing is a technique that removes the sperm from its natural fluid and places it in an artificial fluid that improves sperm motility, longevity, and its ability to penetrate the egg. Some women will become pregnant with one insemination. However, repeat inseminations may be required before proceeding to other alternatives.
In Vitro fertilization (IVF)
 In vitro fertilization (IVF) is an option when various alternatives have failed or are inappropriate. It can be used, for example, in women whose fallopian tubes are either damaged, missing, or diseased.
In vitro fertilization (IVF) is an option when various alternatives have failed or are inappropriate. It can be used, for example, in women whose fallopian tubes are either damaged, missing, or diseased.
The woman is prepared for this procedure with fertility drugs via daily injections. The fertility drugs will stimulate the ovaries to produce many eggs for fertilization and prepare the lining of her uterus to support a pregnancy. The eggs are then taken from her via the transvaginal route, using a needle to aspirate the eggs from the ovary. This is performed under ultrasound guidance in the operating theatre. The eggs collected will be placed in a laboratory dish where they are incubated with her partner’s sperm for about 48 to 72 hours.
Assuming that some eggs are fertilized and continue to develop normally for two days or more, one or more are then transferred via a small hollow catheter into the woman’s uterus. Sometimes, the embryos are transferred on day 5. This is also known as blastocyst transfer. If at least one embryo implants there within about 2 weeks, the woman is pregnant. Pregnancy can be confirmed by urine or blood test. As with other infertility treatments, couples undergoing IVF should recognize that positive outcomes are never guaranteed.
Egg (oocyte) donation can help women who have undergone early menopause or whose ovaries respond poorly to fertility medications. Egg donors can be someone known to the family or an anonymous donor.
Intracytoplasmic Sperm Injection (ICSI)
This is indicated in the following conditions: male infertility problems, failure or poor fertilization during IVF, older women. A single sperm is taken from the male and injected into a single egg from the female. The egg is then placed in a laboratory dish for about 48 to 72 hours. Assuming that some eggs are fertilized and continue to develop normally for two days or more, one or more are then transferred via a small hollow catheter into the woman’s uterus.
Some men have no sperm in the ejaculate but still produce them in the testes. A healthcare provider can remove sperm by placing a needle into the testis or the tubes that drain it. This is called percutaneous epididymal sperm aspiration and testicular sperm extraction (PESA and TESE).
To print a pdf copy, CLICK HERE

[mailerlite_form form_id=3]
Follow at Instagram @obgyn.com.my
