 Vulvovaginal candidiasis is an infection of the vagina caused by a yeast-like fungus (usually Candida albicans). It is one of the commonest causes of vaginitis (inflammation of the vagina). An estimated 75 percent of all women will develop a yeast infection during their lifetime. Vaginal candidiasis infections are very common in pregnancy due to the increased levels of circulating oestrogen in the bloodstream.
Vulvovaginal candidiasis is an infection of the vagina caused by a yeast-like fungus (usually Candida albicans). It is one of the commonest causes of vaginitis (inflammation of the vagina). An estimated 75 percent of all women will develop a yeast infection during their lifetime. Vaginal candidiasis infections are very common in pregnancy due to the increased levels of circulating oestrogen in the bloodstream.
CAUSES
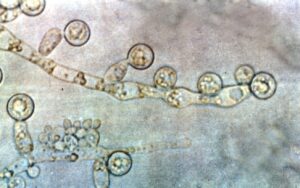
The fungus Candida lives in small numbers in a healthy vagina, rectum and mouth without causing problems. When the vagina’s hormone and pH balance is disturbed, the organisms multiply and cause infections.
 SYMPTOMS AND SIGNS
SYMPTOMS AND SIGNS
- White, “curdy” vaginal discharge, (resembles lumps of cottage cheese). The odor may be unpleasant, but usually not foul-smelling.
- Swollen, red, tender, itching vaginal lips (labia) and surrounding skin.
- Burning sensation on urination.
- Change in vaginal and skin color from pale pink to red (sign of inflammation).
- Pain during sexual intercourse (dyspareunia).
RISK FACTORS
- Pregnancy.
- Combined oral contraceptive pills user.
- Diabetes mellitus.
- Frequent or prolonged antibiotic treatment.
- Reduced immunity from drugs or disease.
POSSIBLE COMPLICATIONS
Without treatment, symptoms may persist and can be extremely uncomfortable. Other infections may co-exist, especially bacterial. About 5 percent of women with vulvovaginal candidiasis may develop recurrent vulvovaginal candidiasis (RVVC), which is defined as four or more episodes of vulvovaginal candidiasis in the previous year. Recurrent or persistent infection is usually due to the non-albicans species. During pregnancy, vaginal candidiasis has no impact on the pregnancy outcome or the fetus.
INVESTIGATION
Diagnostic tests may include laboratory studies of vaginal discharge, cervical cytology smear (Thin Prep) and pelvic examination.
 DIAGNOSIS
DIAGNOSIS
Diagnosis is often made clinically, from the presenting complaints and the typical appearance of the discharge seen during speculum (internal) examination of the vagina. The smear of the discharge for laboratory identification is sent if the diagnosis is uncertain or if the symptoms persist despite the completion of therapy. The identification of the candida is sometimes seen in the Thin Prep or Pap smear report.
TREATMENT
- Drug therapy with antifungal drugs, either in vaginal creams or suppositories or in oral form, is usually recommended. During pregnancy, vaginal cream or tablet suppositories are preferred.
- If vaginal creams or suppositories are prescribed, use a panty liner during the treatment period to avoid the discharge from staining the undergarment.
- It is best not to do self-treatment for the disorder until the specific cause of your vaginal infection is determined. Studies have shown that as many as two-thirds of all non-prescription drugs sold to treat vulvovaginal candidiasis were used by women without the disease.
- Do not douche unless prescribed for you.
- For severe infections, repeated doses may be given, or the duration of treatment may be longer.
- Recurrent vulvovaginal candidiasis treatment usually involves one to two weeks of intensive anti-fungal medication, followed by up to six months of a lower “maintenance” dose.
- There is no evidence to show that treatment of sexual partner will reduce the recurrence of the infection. Therefore, routine treatment of male partner is not required unless the partner has symptoms attributed to candida infection.
- It is advisable to avoid sexual intercourse until symptoms cease.
 PREVENTIVE MEASURES (for those with recurrent infections)
PREVENTIVE MEASURES (for those with recurrent infections)
- Keep the genital area clean. Use an unscented, dermatologically approved, soap-free skin cleanser. Use it once or twice a day during shower. Do not wash too frequently with normal bath soaps or shower foams.
- Consider other family planning methods if you have recurrent candida infection and currently on the combined oral contraceptive pills.
- Take showers rather than tub baths.
- Wear cotton underpants or pantyhose with a cotton crotch. Do not wear underwear at night.
- Do not sit around in wet clothing, especially a wet bathing suit.
- Limit your intake of sweets and alcohol.
- After urination or bowel movements, cleanse by wiping or washing from front to back only in one direction (vagina to anus).
- Lose weight if you are overweight.
- If you have diabetes, ensure good sugar control.
- Avoid unnecessary use of antibiotics unless prescribed by the doctor.

- There are many feminine hygiene products in the market, many of which can irritate the vulva and vagina: such as special sanitary pads, feminine spray, douches and deodorants, scented oils, bubble baths, bath oils, talcum powder etc. These should be avoided.
- There is no strong evidence to support the routine advice of eating yogurt or a low sugar diet in those with recurrent or persistent yeast infection. However, some women may find it beneficial and there is no harm in trying it out if you are keen. It is a healthy practice anyway. The benefits of taking probiotics in recurrent or persistent yeast infection is also uncertain but there is probably no harm if you are keen to start on it.
To print a pdf copy, click HERE







