It is an abnormal growth of cells in the muscle layer (myometrium) of the uterus. Uterine fibroids are common and usually benign (not cancerous). Fibroids range in size from very tiny to the size of an orange or larger.
INCIDENCE
Uterine fibroids are the most common pelvic growth in women. The actual incidence among all women is unknown but generally cited as 20 to 25 % in the general population and is highest between age 35 to 45 years old.
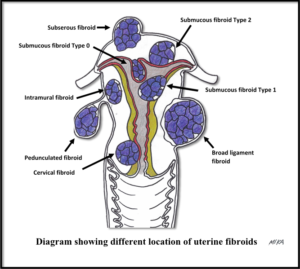
TYPES (based on location in the uterus)
- Subserous which appear on the outside of the uterus.
- Intramural, which is confined to the wall of the uterus.
- Submucous which appears inside the uterus.
- Pedunculated fibroids, which are attached to the uterine wall by stalks.
- Broad ligament type which grows to the side of the uterus
- Cervical type, which is rare.
SYMPTOMS AND SIGNS
- Some may not notice it (no symptoms). Therefore, this may only discover on abdominal or pelvic examination.
- Frequent menstruation, with possibly heavy bleeding, occasionally with large clots and need to change pads often. There may be associated with pain.

- Prolonged menses or bleeding between periods.
- Pressure symptoms – feelings of pressure on the urinary bladder, rectum or spine. Pressure on the bladder will cause frequent urination.
- Progressive swelling in the lower abdomen or may be able to feel a lump in this area.
- Anemia (weakness, fatigue, and paleness) due to excessive menstrual bleeding.
- Infertility (difficulty in conceiving)
- Painful sexual intercourse or bleeding after intercourse (rare).
In many women, more than one fibroid is usually present.
CAUSES
The exact cause is unknown. Oestrogen is required for their stimulation and growth, as fibroids are rare in prepubertal girls. In postmenopausal women, the fibroid size will shrink over time.
RISK FACTORS
- Genetic factors may play a role – for example, fibroids are 3 to 5 times more common in black women than in white women.
- Family history of fibroids.
- Age (older women are at higher risk than younger women).
- No history of pregnancy before.
- Diet high in fat and/or obesity may be a risk.
PREVENTIVE MEASURES
It cannot be totally prevented at present. Factors that may lower your risk of fibroids are:
- Pregnancy (the risk decreases with an increasing number of pregnancies)
- Long-term use of hormonal contraceptives (oral or injectables).
POSSIBLE COMPLICATIONS
- Heavy bleeding and anemia.
- Complications can occur in pregnancy such as spontaneous miscarriage (usually associated with the submucous fibroids type), premature labor (usually associated with large fibroids), and placental separation (abruption) may occur when the placenta overlies the fibroids. With a large fibroid, foetal growth may be at risk because blood flow is diverted from the fetus to the fibroid.
- Recurrence of fibroids following surgery to remove them.
- Pelvic pain if they outgrow their blood supply (called degeneration). Pain lasts days to a week or more.
- Malignant change in the fibroids (occurs in less than 0.5%). This rare complication is usually signaled by very rapid growth.
INVESTIGATIONS
Diagnostic tests may include:
- Laboratory blood studies – full blood count to exclude anaemia due to excessive blood loss
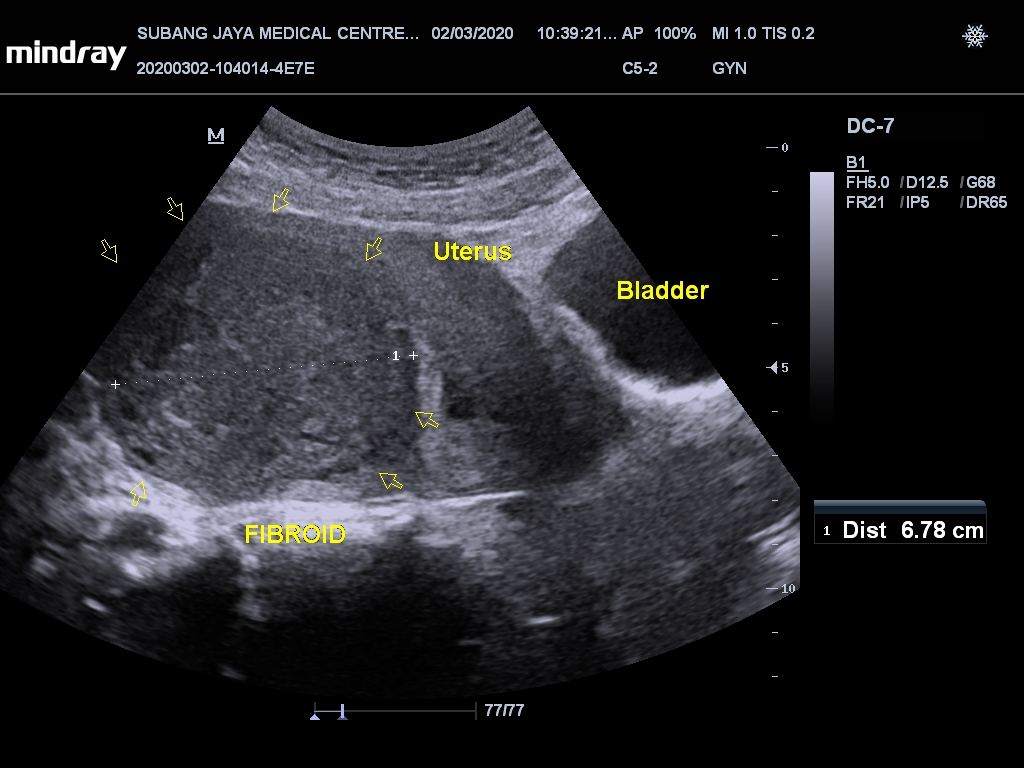
- Ultra-sound scan of the uterus.

- Hysteroscopy (a telescopic instrument is inserted through the vagina to look inside the uterus) to diagnose the submucous type and look for other causes of bleeding
- Saline infusion sonohysterography (ultrasound scan of the uterus after instillation of fluid into uterine cavity). This is helpful in diagnosing the different type of submucous fibroids
- Magnetic Resonance Imaging (MRI) – sometimes, the ultrasound scan findings may be confused with adenomyosis and both may also co-exist. In such a situation, MRI of the pelvis may be necessary and is a better way of localizing and characterizing the fibroids. This is also necessary if planning for uterine artery embolization (UAE) treatment.
- Endometrial biopsy – to exclude cancerous change. This can be done either in the clinic or in operating theatre (endometrial curettage).
TREATMENT
- Treatment is not required if there are no symptoms attributed directly to the fibroids or if the symptoms are mild and can be controlled with medications.
- Medication can help ease the symptoms but will not cure fibroids.

- A non-steroidal anti-inflammatory drugs (such as diclofenac, ibuprofen, mefenamic acid) is given if there is associated period pain with heavy flow.
- Birth control pills (combined oral contraceptives) can reduce flow by 30 to 40% and suitable for those who required family planning as well.
- Tranexamic acid tablets can help in reducing the monthly heavy flow by up to 40%. It is taken only during your heavy bleeding days and usually for 2 to 4 days.
- Iron supplements is given if you are anaemic from excessive blood loss.
- A gonadotropin-releasing hormone may be given in those with excessive bleeding or while waiting for surgery. It will induce abrupt, artificial menopause that will stop the bleeding and reduce the size of the fibroid. In general, this therapy is not used for longer than 3 months and is usually given prior to surgery. Another agent that can reduce the size of the fibroids and relieve the symptoms is ulipristal acetate (ESMYA). However, this is no longer used now due to its liver toxicity.

- Fibroids can be removed surgically when they cause excessive bleeding or pain, produce symptoms that interfere with conception or pregnancy. Several surgical options are available. Hysterectomy is surgery to remove the uterus; a myomectomy removes only the fibroids.
- A non-surgical option is the Uterine fibroid embolization (UFE), also called uterine artery embolization (UAE). It is a procedure that treats all fibroids in the uterus by cutting off the blood flow (embolize).
- Blood transfusions may be needed to correct anemia, before, during or after the surgery.

- Treatment should be individualized, depending on symptoms and diagnostic tests, location and size of the fibroids, your general health and desire for future pregnancies.
- For minimal symptoms, no treatment may be needed, and you will be re-examined at 3-6 months intervals. Keep a record of dates of bleeding and the number of pads used each day.
- There is no special diet for women with fibroids. Consider a weight loss diet if obesity is a problem.
- Fibroids usually decrease in size without treatment after menopause. However, it will not totally disappear.
To download this article in pdf, CLICK HERE
CLICK HERE to view images of gross specimens of fibroids after surgical removal