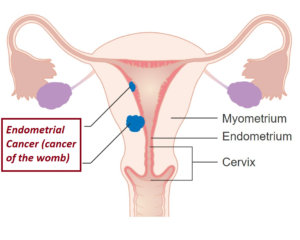
 Endometrial hyperplasia is an overgrowth of endometrial tissue (which is the inner lining of the uterus which shed every month as menstrual blood flow). It is not cancerous. However, there is a form of severe hyperplasia which can be precancerous (especially when there is presence of abnormal cells called atypia). Classification of the hyperplasia includes:
Endometrial hyperplasia is an overgrowth of endometrial tissue (which is the inner lining of the uterus which shed every month as menstrual blood flow). It is not cancerous. However, there is a form of severe hyperplasia which can be precancerous (especially when there is presence of abnormal cells called atypia). Classification of the hyperplasia includes:
- simple or complex (adenomatous) hyperplasia without atypia, or
- simple or complex (adenomatous) hyperplasia with atypia.
Patients who have endometrial hyperplasia without atypia usually respond well to progestogen therapy and are not at increased risk for uterine cancer. The progression of hyperplasia to endometrial cancer increases as the abnormal cells (atypia) of the hyperplasia develops.
Symptoms and signs
- Abnormal menstrual bleeding such as bleeding between normal menstrual periods, heavy and/or prolonged menstrual bleeding
- Irregular menstrual cycles, with heavy menstrual bleeding
- Post-menopausal bleeding
Causes
 Endometrial hyperplasia develops when there is a chronic oestrogen stimulation (a female hormone) of the endometrium relative to the amount of progesterone (another female hormone). This excess may arise from within the body or from the use of hormone-containing medications. Tamoxifen, a drug used for breast cancer, is associated with increased risk of endometrial hyperplasia.
Endometrial hyperplasia develops when there is a chronic oestrogen stimulation (a female hormone) of the endometrium relative to the amount of progesterone (another female hormone). This excess may arise from within the body or from the use of hormone-containing medications. Tamoxifen, a drug used for breast cancer, is associated with increased risk of endometrial hyperplasia.
Risk factors
- Women with irregular menstrual cycles (especially I those with anovulatory cycles, meaning menstrual cycle without the occurrence of ovulation), polycystic ovary syndrome (PCOS) and those on oestrogen replacement therapy without progestogen administration.
- Diabetes.
- Obesity.
- Women who are around menopause age (perimenopausal).
- Heavy or abnormal menstrual bleeding in premenopausal women.
- Medications – such as tamoxifen.
 Possible complications
Possible complications
- Without treatment, there is a higher risk for endometrial cancer for women with hyperplasia in the presence of atypia features.
- Excessive, uncontrollable bleeding leading to anaemia
Investigations
Investigations will include laboratory studies, such as blood tests to check for anaemia and cervical cytology smear (Thin Prep). In addition, an abdominal or a vaginal pelvic ultrasound scan, an endometrial biopsy with or without a hysteroscopy (use of a telescopic instrument inserted through the vagina to look inside the uterus) may be performed for a definitive diagnosis of the type of hyperplasia and to rule out cancer.
Treatment
 Treatment will be individualized based on the investigation findings, your age, and your reproductive desires. Medication is normally the first step in treatment. Progestogen tablets are the most prescribed for this. Combined oral contraceptive pills can be used if there is an additional need for pregnancy prevention. The aim of treatment is to cause the lining to shed and prevent it from building up again. It is often given cyclically (for several cycles) and will cause regular withdrawal menstrual bleeding. The progestogen can be given continuously for several months but this tends to cause irregular bleeding. Repeat endometrial biopsy and possibly other tests will be used to follow up this condition. Follow-up is important to correct any of the underlying abnormalities that can cause the hyperplasia to recur again. In most cases, hormonal treatment with medications (oral or injectables) will reverse the hyperplasia caused by excessive oestrogen. Alternatively, an intrauterine device containing a progestogen (MIRENA) can be inserted.
Treatment will be individualized based on the investigation findings, your age, and your reproductive desires. Medication is normally the first step in treatment. Progestogen tablets are the most prescribed for this. Combined oral contraceptive pills can be used if there is an additional need for pregnancy prevention. The aim of treatment is to cause the lining to shed and prevent it from building up again. It is often given cyclically (for several cycles) and will cause regular withdrawal menstrual bleeding. The progestogen can be given continuously for several months but this tends to cause irregular bleeding. Repeat endometrial biopsy and possibly other tests will be used to follow up this condition. Follow-up is important to correct any of the underlying abnormalities that can cause the hyperplasia to recur again. In most cases, hormonal treatment with medications (oral or injectables) will reverse the hyperplasia caused by excessive oestrogen. Alternatively, an intrauterine device containing a progestogen (MIRENA) can be inserted. 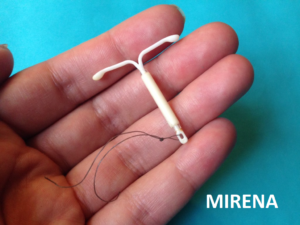 It can be used to treat and prevent the development of hyperplasia. It is a form of contraceptive as well and lasts for 5 years. After 5 years, it should be removed and a new one inserted if necessary for the same purpose. The outcome of treatment is often excellent. However, in some women, a hysterectomy (surgery to remove the uterus) may be required, particularly when hormone therapy has failed or when precancerous cells are discovered.
It can be used to treat and prevent the development of hyperplasia. It is a form of contraceptive as well and lasts for 5 years. After 5 years, it should be removed and a new one inserted if necessary for the same purpose. The outcome of treatment is often excellent. However, in some women, a hysterectomy (surgery to remove the uterus) may be required, particularly when hormone therapy has failed or when precancerous cells are discovered.
Activity
No restrictions unless you have surgery. Then resume your activities gradually. You may resume sexual relations once bleeding has stopped or medical clearance is given.
Diet
Usually, no special diet is required. If you are overweight, weight reduction is important and helps to reduce the chance of recurrence.
Prevention
- Women who have less than 4 menstrual cycles a year should see their doctor and take medications to shed the menstrual lining (endometrium). Medications should be taken every 1 to 3 months to induce withdrawal bleeding. This helps to prevent the development of endometrial hyperplasia and uterine cancer.
- If taking oestrogen, balance it with the right amount of progestogen.
- Appropriate weight – aim for weight loss if obesity is a problem.
- Birth control pills (oral contraceptives) contain oestrogen along with a form of progestogen. The pills may help protect against endometrial hyperplasia in women who do not have regular periods. It has added advantage of providing contraception
To print a pdf copy, Click HERE
[mailerlite_form form_id=3]