Cervical intraepithelial neoplasia (or CIN) refers to the presence of abnormal cells seen on the cervical cytology smear. These abnormal cells are obtained from the lining of the outer cervix and can range from mild to severe changes. A diagnosis of CIN changes is not cancer. However, the severe form of dysplasia can be considered a precancerous condition and may eventually progress to cancer in several years if not treated.
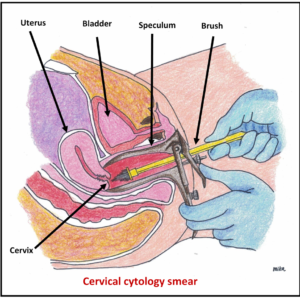
The cervical cytology smear was previously referred to as Pap smear. Currently, the newer cervical cancer screening uses a liquid based cytology and the commonest one used are: Thin Prep or Sure-Path. These are better and more accurate compared to the conventional Pap smear test.
Classification of CIN
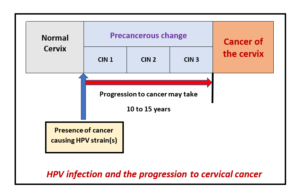
 CIN is divided into 3 groups, which is CIN I, II and III. This is based on the severity of the cell changes (dysplasia). CIN III refers to abnormal cells that involve the whole thickness of the surface lining of the outer cervix and has the highest chance of further progression to cancer.
CIN is divided into 3 groups, which is CIN I, II and III. This is based on the severity of the cell changes (dysplasia). CIN III refers to abnormal cells that involve the whole thickness of the surface lining of the outer cervix and has the highest chance of further progression to cancer.
Symptoms and signs.
 Most women do not have any symptoms. The diagnosis is often made from the routine cervical cytology screening (Thin Prep or Sure-Path). Some women may have abnormal vaginal bleeding. Occasionally, there may be excessive vaginal discharge or bleeding after sex.
Most women do not have any symptoms. The diagnosis is often made from the routine cervical cytology screening (Thin Prep or Sure-Path). Some women may have abnormal vaginal bleeding. Occasionally, there may be excessive vaginal discharge or bleeding after sex.
Causes
There is an association with human papillomavirus (HPV). The HPV is found in 99% of cervical cancer. The HPV is usually acquired from sexual intercourse. Majority of HPV infection will disappear on its own. Only up to 10% of the infections are persistent and the progression to cervical cancer may take 10 to 15 years to developed.
 Risk Factors
Risk Factors
- History of infection with the human papillomavirus (HPV), which may also cause genital warts. In the presence of HPV infection, smoking, use of combined oral contraceptive pills and a decrease in immune response (eg HIV infection, illness or on chemotherapy) are associated with an increased risk of precancerous (CIN) change in the cervix
- Multiple sexual partners.
- Early age of first sexual intercourse (before age 18).
- Daughters of women who took diethylstillbestrol (DES) during pregnancy.
Prevention
- Vaccination against HPV infection – currently, there are two vaccines available for this purpose (Gardasil and Cervarix).
- Sexual monogamy of both partners.
- Regular cervical smears – this will not prevent dysplasia but will be able to detect it early. Treatment of dysplasia will prevent the development of cancer of the cervix.
- Do not smoke.
- Use of a diaphragm by the female or a condom by the male during sexual intercourse.
Complications 
Severe dysplasia may progress to cancer of the cervix.
Investigations and diagnosis
- Cervical smear (liquid based cytology such as Thin Prep or Sure-Path)

- HPV DNA (virus study) test – the procedure to do this test is similar to cervical smear and can be done concurrently with the liquid based cytology.
- Colposcopy – this is a microscopic examination of the cervix, vagina or vulva. It is used to diagnose potential abnormalities of these areas, which sometimes cannot be seen with the naked eyes. The colposcope can magnify the tissue by up to 30 times, thus making it clearer and much more accurate in terms of surface evaluation. Therefore, the biopsy of the abnormal areas performed with a colposcopic examination is more accurate than those done without the use of a colposcope. A stain or other chemical agent is applied so that the abnormal areas will become more prominent and easily seen.

Colposcopy Machine Biopsy will be taken if necessary and sent for histological examination. If a biopsy is done or endocervical curettage is performed, these procedures may cause some cramping or bleeding. Click HERE to read more about colposcopy.
Treatment
- Spontaneous regression (reversal) does occur in a significant number of patients, especially those with mild dysplasia (CIN I). Therefore, a period of observation and follow-up may be advised in those with only CIN I changes.
- Treatment measures will vary depending on the degree and extent of the cervical dysplasia following the colposcopic evaluation and the biopsy report. Possibilities include cryotherapy (freezing), laser surgery, loop excision of the cervix or cone biopsy.

- These procedures can be performed in the clinic setting, but most centres do it either as a daycare or an overnight stay. It does not cause pain and the recovery is quick. You will have vaginal bleeding for a few days, followed by watery and bloody discharge over the next 2 to 3 weeks.
- If surgical treatment to the cervix is performed, you should delay sexual relations, avoid soaking in bathtub, swimming or use of tampons and douches for 2 to 3 weeks. You can shower as usual. Please discuss this with your doctor.
- The outlook is excellent if the abnormal areas are completely removed. Sometimes, the margins of the removed cervical tissue may show abnormal cells (dysplasia), thus signifying incomplete excision. This can be treated either with a repeat procedure such as loop excision or a cold knife cone biopsy. Alternatively, the woman may opt for a hysterectomy, especially if she has completed childbearing,
- Rarely, complications can result from the treatment, such as excessive bleeding or infection.
- Follow-up care will depend on the treatment method used and whether the margins are clear of the abnormal cells.
- Follow-up cervical smears every 6 months, for 1 to 2 years, may be recommended to verify the success of treatment and to detect any recurrence. Additional screening for the HPV DNA virus may be done following surgical treatment and this may be of use to decide further management and follow-up schedule. Please discuss the screening intervals with your doctor, depending on the repeated cervical smear and whether the HPV DNA virus is negative.
- HPV vaccination following the treatment of CIN lesion by loop excision of the cervix will only provide protection against future exposure of other HPV strains. It will not change or alter the natural course of the current HPV strain(s) causing the infection, which may still be present in the cervix even after treatment. The recurrence of CIN may still be caused by the pre-existing HPV strain(s) prior to the vaccination. Therefore, it is important to continue follow-up with regular cervical smears.

- It is heartening to know that no women should die of cervical cancer now because it is totally preventable. Mass vaccination of young schoolgirls and boys prior to their first sexual activity with HPV vaccination will reduce the infection rate. Improvement in detection of abnormal cells and HPV in the cervix have enable earlier treatment for the detection and treatment precancerous change, thus preventing further progression to cancer of the cervix.
See your doctor immediately if there is:
- Excessive vaginal bleeding which soaks more than 1 pad each hour.
- Persistent and abnormal vaginal discharge.
- Signs of infection, including headache, muscle aches, dizziness or a general ill feeling and fever.
To download and print a pdf copy, CLICK HERE
Please subscribe HERE to receive the regular newsletter and get the latest updates regarding Women’s Health