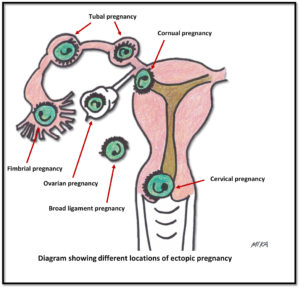
Ectopic pregnancy is one that develops outside the uterus. The egg (oocyte) and the sperm meet in the fallopian tube and fertilization occurs. The embryo is supposed to move back to the uterine cavity for implantation. However, in ectopic pregnancy this does not occur, and the embryo gets implanted elsewhere. The most common location is in one of the narrow tubes that connect each ovary to the uterus (fallopian tube). As the fertilized egg enlarges, the fallopian tube stretches and ruptures, causing life-threatening internal bleeding. Other locations include the ovary, cervix, space beside the uterus (broad ligament space) or in the abdominal cavity. About 1 in 100 pregnancies is an ectopic.
The most common location is in one of the narrow tubes that connect each ovary to the uterus (fallopian tube). As the fertilized egg enlarges, the fallopian tube stretches and ruptures, causing life-threatening internal bleeding. Other locations include the ovary, cervix, space beside the uterus (broad ligament space) or in the abdominal cavity. About 1 in 100 pregnancies is an ectopic.
CAUSES AND RISK FACTORS
The occurrence of ectopic pregnancy is usually associated with an abnormal function of the fallopian tubes. Hence, tubal pregnancy is the most common type. Hormonal imbalances or abnormal development of the fertilized egg might also play a role. Certain condition may predispose to a higher chance of ectopic pregnancy such as:
- Previous abdominal or pelvic infection
- Pelvic inflammatory disease (PID), involving the fallopian tubes
- Pregnancy after tubal ligation
- Assisted reproduction techniques such as in vitro fertilization.
- Adhesions (bands of scar tissue) from previous pelvic surgery.
- Previous tubal pregnancy.
- History of endometritis (infection of the inner uterine lining)
- Malformed (abnormal) uterus or fallopian tubes
- Pregnant with an intrauterine device (IUD) in place (failure of IUD)
SIGNS AND SYMPTOMS
- Early stages: it is just like any other pregnancy symptoms – such as a missed menstrual period or any menstrual irregularity, frequent urination, nausea, breast tenderness. As the embryo and sac enlarges, the following symptoms may be present:
- Light vaginal spotting or bleeding
- Lower abdominal pain and cramps
- Fainting spells
- Pain in the shoulder (rare)

- Late-stage is when the ectopic pregnancy ruptured and causes continuous bleeding: symptoms will be sudden, sharp, severe abdominal pain, dizziness, fainting and shock (paleness, rapid heartbeat, drop in blood pressure and cold sweats). This is a dire emergency and immediate surgery is required.
PREVENTIVE MEASURES
It cannot be totally prevented. Many women who are diagnosed with an ectopic pregnancy do not have a recognizable risk factor. Early consultation with your doctor is important if you are pregnant because ectopic pregnancy can be diagnosed early before complications arise.
EXPECTED OUTCOME
An ectopic pregnancy cannot progress to full term or produce a viable  fetus. Rupture of an ectopic pregnancy is an emergency requiring immediate treatment. Full recovery is likely with early diagnosis and surgery. Subsequent pregnancies are normal in about 50 to 85% of patients.
fetus. Rupture of an ectopic pregnancy is an emergency requiring immediate treatment. Full recovery is likely with early diagnosis and surgery. Subsequent pregnancies are normal in about 50 to 85% of patients.
POSSIBLE COMPLICATIONS
- Anaemia due to blood loss
- Diminished fertility.
- Shock and death from internal bleeding.
- Infection
INVESTIGATIONS
Diagnostic tests may include:

- Laboratory blood studies such as full blood count to rule out anaemia
- Ultrasound scan of the pelvis – either a trans-abdominal or a trans-vaginal ultrasound is done. The trans-vaginal scan involves inserting a special wand-like instrument into your vagina to look for the gestational sac in the uterine cavity. In ectopic pregnancy the uterus is empty (absent sac). And other findings may include:
- fluid (blood) outside the uterus
- an abnormal mass adjacent to the uterus
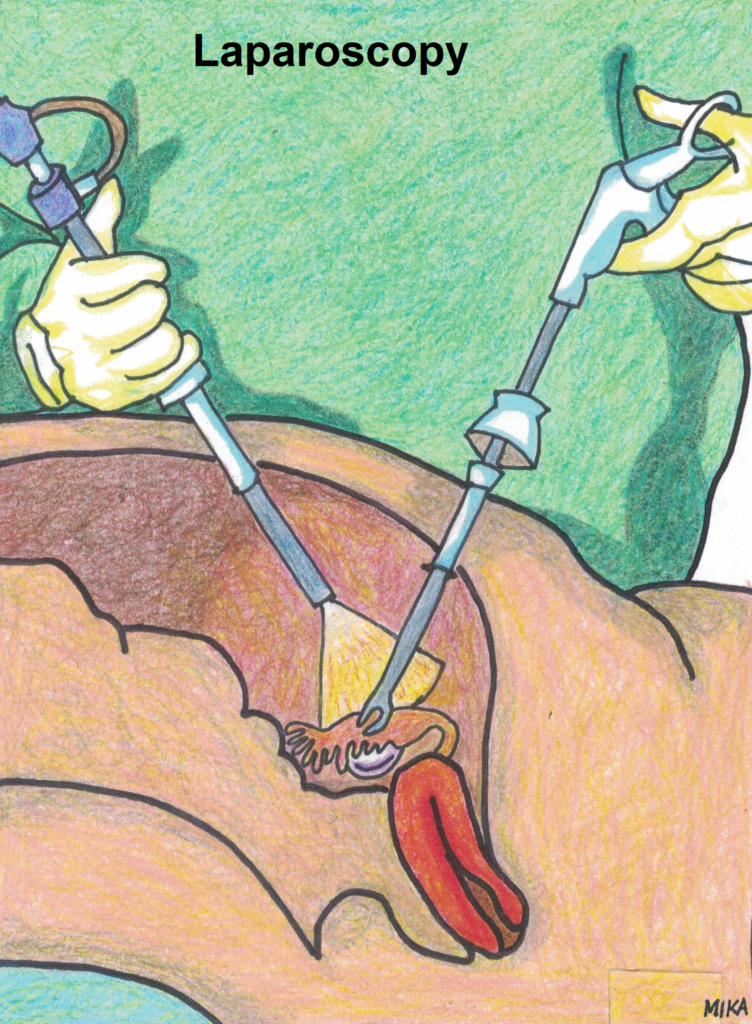
- Laparoscopy (telescopic instrument with fibre optic light is inserted into the abdomen for visual examination and may be used to remove the ectopic pregnancy).

- Serial measurement of pregnancy hormone serum hCG or progesterone – ectopic is suspected if these shows abnormal levels over the course of a few days and with an absent gestational sac in the uterus on ultrasound scan
TREATMENT
- The treatment of ectopic pregnancy is to remove the pregnancy. If it is in the tube, sometimes the affected tube may need to be removed together. It can be done either via laparoscopy or open surgery (laparotomy). Laparoscopy is the best surgical method. It is minimally invasive and offers quicker recovery time and less post-operative pain.

- Intra or post-operative blood transfusion may be given, depending on the amount of blood loss.
- Future pregnancy is possible with one fallopian tube. If the tubal pregnancy has not ruptured and is not seriously damaged, it may be possible to conserve the tube by removing only the ectopic pregnancy tissues.
- Post-operatively, pain relief medication is given for 2 to 7 days. Antibiotics is usually not necessary.
- Iron supplements for 1 to 2 months is necessary if the haemoglobin is low or there is excessive bleeding.
- Avoid sexual relations until a follow-up medical examination determines healing is complete. You should discuss with your doctor regarding various contraceptive options if you are not keen or wishes to delay future pregnancy. If you are keen for the next pregnancy, it is prudent to wait for at least 2 to 3 months before trying again.
- There is no specific dietary restriction.
- In a situation whereby the tube has been conserved, there is some risk that some of the pregnancy tissues may remain in the tube. Weekly blood tests to check pregnancy hormone levels (hCG) may be recommended until they are negative to rule out this possibility. If it is still persistent, some ectopic pregnancy tissue has been retained and medication (methotrexate, which is a chemotherapy drug) is usually given until the levels become normal.
- In some early, unruptured, or chronic ectopic pregnancies, methotrexate has been used to treat the ectopic pregnancy. Specific guidelines and close follow-up are necessary when this drug is prescribed.
- Many women who have had an ectopic pregnancy will be able to get pregnant again. Some may have difficulty becoming pregnant again due to underlying risk factors discussed early. Assisted reproductive technology (ART) is an option for them.
 SEE YOUR DOCTOR IF:
SEE YOUR DOCTOR IF:
- You develop signs of infection such as headache, muscle aches, dizziness or a general ill feeling and fever
- You have excessive vaginal bleeding which soaks more than 1 pad or tampon each hour
- You experience abdominal swelling or pain, with poor oral intake
- Increasing pain, swelling, redness, discharge or bleeding in the surgical area.
- The urge to urinate frequently, especially if associated with pain and abnormal urine colour
- Persistent and abnormal vaginal discharge
To download a pdf copy, CLICK HERE
To watch a laparoscopic view of an ectopic pregnancy (tubal pregnancy), CLICK HERE