Most women stay in the hospital for 24 to 48 hours after giving birth (or 3 to 4 nights after a caesarean section). This will depend on the condition of the mother and baby.
Most women stay in the hospital for 24 to 48 hours after giving birth (or 3 to 4 nights after a caesarean section). This will depend on the condition of the mother and baby.
The physical changes that occur with pregnancy usually resolve by the end of 6 weeks, although some may resolve much earlier than this. It is important to know all these changes, as it will help you cope better and lessen your worries. Emotional sup¬port and much needed help from your spouse and family members is equally important to assist you in facing these changes and coping with the arrival of a new member into the family. You will also get lots of advice from friends and relatives who visit you – some may be conflicting and may be harmful. There are many ways of doing things with no particular hard and fast rules on what is best for you. It is best to avoid traditional or Chinese herbs during this period. In the end, it is all boils down to common sense and you have to decide what is best for you and your baby. Do some reading and ask your doctor or midwife about your recovery during the postnatal period
1. PAIN
Pain after childbirth is to be expected and usually tolerable. Fortunately, this is only for a few days and responds well to simple oral pain-killers. The pain is due to the uterine contractions when the uterus contracts back to its normal size and helps to reduce the blood loss. The genital area may be painful or sore, especially if there is stitching resulting from either an episiotomy or a tear. Inform your healthcare provider if you have significant pain so that a stronger painkiller medication can be given. For relief of discomfort caused by the episiotomy, use warm-water cleansing and salt-water bath (10 to 20 minutes, two to three times a day in water 10 cm deep in the tub). This can also help in the healing process.
2. SWELLING AND SWEATING
 Following a vaginal delivery, some mother may discover that their body and face looks slightly swollen. This is quite normal. The intense pushing efforts during delivery may cause their face, neck and legs to swell, but this should go away after a few days or up to two weeks. The area outside the vagina may also swell, due to prolonged pushing and straining. Ice packs are useful to reduce the swelling and offer relief. Some women following Caesarean delivery may also notice that their lower limbs will be slightly swollen. This is normal, provided there is no associated pain and tenderness over the calf area. You may notice that you tend to sweat more and often drenched in sweat. This is very common and is due to the sudden decrease in hormone levels after delivery. It is quite similar to the night sweats and hot flashes that menopausal women start to encounter in their late forties.
Following a vaginal delivery, some mother may discover that their body and face looks slightly swollen. This is quite normal. The intense pushing efforts during delivery may cause their face, neck and legs to swell, but this should go away after a few days or up to two weeks. The area outside the vagina may also swell, due to prolonged pushing and straining. Ice packs are useful to reduce the swelling and offer relief. Some women following Caesarean delivery may also notice that their lower limbs will be slightly swollen. This is normal, provided there is no associated pain and tenderness over the calf area. You may notice that you tend to sweat more and often drenched in sweat. This is very common and is due to the sudden decrease in hormone levels after delivery. It is quite similar to the night sweats and hot flashes that menopausal women start to encounter in their late forties.
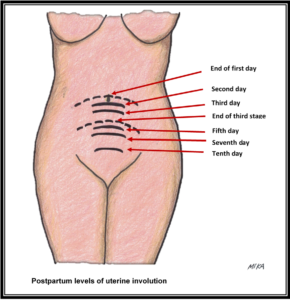
 3. UTERUS
3. UTERUS
Following the delivery of the baby and the placenta, the uterus will immediately contract. During the third stage, an injection will be given intramuscularly to help the uterus to contract to reduce bleeding. You may feel cramps in your lower abdomens due to this. Your uterus size will still be quite large. You can feel it at the level or slightly above your belly button. It can be painful to touch. Over the next few days, the size will gradually reduce and you will still feels the cramps, especially when you are breastfeeding. After two weeks, the uterus will be down into your pelvis and back to pre-pregnancy size by 3rd to 4th week. This process is called involution of the uterus.
4. WEIGHT
 New mothers generally lose 5 to 6 kg with the baby’s birth and another 1 to 2 kg in the first few days after delivery. Additional weight loss continues for 6 to 8 weeks when you should be back to normal weight. Breast-feeding mothers usually have a more dramatic weight loss than non-nursing mothers.
New mothers generally lose 5 to 6 kg with the baby’s birth and another 1 to 2 kg in the first few days after delivery. Additional weight loss continues for 6 to 8 weeks when you should be back to normal weight. Breast-feeding mothers usually have a more dramatic weight loss than non-nursing mothers.
5. DIET
In general, there is no specific dietary restriction. Unfortunately, Asian cultures have a long list of food restrictions and taboos, which has no scientific basis for it. Use your common sense to decide what is best for you and your baby. Discuss this with your doctor if you are not sure. This is an important period when you need a proper diet to help you to recover and to ensure successful breast-feeding. Therefore, you should aim for a healthy and balanced diet. If you are breastfeeding, do avoid alcohol, and smoking. Drinks plenty of fluids. You should drink at least a glass full or more fluids after each feeding. This is to avoid dehydration, which can affect milk production.
6. BOWEL MOVEMENTS & URINATION
 It may take several days before the first postpartum bowel movement occurs. Furthermore, constipation is not uncommon during pregnancy. In many women, there is a psychological fear that the bowel movement will be painful and tear stitches. Try not to worry; eat a high-fiber diet; drink plenty of fluids and start a mild exercise routine. Sometimes, haemorrhoids may developed, which is a distention of blood vessels at the entrance to your anus. Try to avoid straining because this can make it worse. Special ointment may help to relieve the discomfort due to haemorrhoids. A stool soften¬er laxative such as lactulose or macrogol will be helpful. If narcotic pain medicines are used, they can sometimes cause constipation.
It may take several days before the first postpartum bowel movement occurs. Furthermore, constipation is not uncommon during pregnancy. In many women, there is a psychological fear that the bowel movement will be painful and tear stitches. Try not to worry; eat a high-fiber diet; drink plenty of fluids and start a mild exercise routine. Sometimes, haemorrhoids may developed, which is a distention of blood vessels at the entrance to your anus. Try to avoid straining because this can make it worse. Special ointment may help to relieve the discomfort due to haemorrhoids. A stool soften¬er laxative such as lactulose or macrogol will be helpful. If narcotic pain medicines are used, they can sometimes cause constipation.
 You may have painful urination. On the first day, you may not feel any urge, or an urge with no urination. This is a result of bladder and urethra compression when the baby’s head and body descent through the vagina. The surrounding tissues area at the opening to the urethra is often swollen and sore after vaginal delivery. It is important to urinate within 6 to 8 hours after vaginal delivery to avoid infection. Getting up and moving can help. If you are unable to urinate on your own, the nurse may insert a small urinary catheter (a thin, flexible plastic tube) through the urethra into the bladder to drain the urine. This is usually seen in those who had epidural or underwent difficult instrumental delivery (either forceps or vacuum). Your ability to micturate on your own should return to normal after 24 hours. From then onwards, there will be an increase in urine volume and frequency as the excess body fluids from the pregnancy is excreted. In some women, there may be urinary leakage when they laugh, cough or sneeze. This is called urinary incontinence and should improve with time. In some cases, the recovery may take several months. You should discuss with your midwife or doctor regarding pelvic floor exercises (Kegel) to manage this problem.
You may have painful urination. On the first day, you may not feel any urge, or an urge with no urination. This is a result of bladder and urethra compression when the baby’s head and body descent through the vagina. The surrounding tissues area at the opening to the urethra is often swollen and sore after vaginal delivery. It is important to urinate within 6 to 8 hours after vaginal delivery to avoid infection. Getting up and moving can help. If you are unable to urinate on your own, the nurse may insert a small urinary catheter (a thin, flexible plastic tube) through the urethra into the bladder to drain the urine. This is usually seen in those who had epidural or underwent difficult instrumental delivery (either forceps or vacuum). Your ability to micturate on your own should return to normal after 24 hours. From then onwards, there will be an increase in urine volume and frequency as the excess body fluids from the pregnancy is excreted. In some women, there may be urinary leakage when they laugh, cough or sneeze. This is called urinary incontinence and should improve with time. In some cases, the recovery may take several months. You should discuss with your midwife or doctor regarding pelvic floor exercises (Kegel) to manage this problem.
 7. BATHING
7. BATHING
You may shower and shampoo at any time after delivery, as long as you are steady on your feet. You should continue to do so while at home to ensure cleanliness and to avoid infection to you and your baby. You should dry the stitched area (either Caesarean or perineal wound) gently with a clean and soft towel after each shower.
8. BREASTS
The milk “comes in” on the third or fourth postpartum day and there is some initial discomfort with the engorge¬ment and fluid retention (edema) in the breasts along with milk leakage. Nursing mothers will have instructions on how to initiate the breast-feeding process while in the hospital.
For non-nursing mothers, the engorgement will start to decrease after 2 to 3 days. Pain and discomfort can be eased with the use of ice packs, mild pain medicine and wearing a support bra. Special drugs to sup¬press lactation are not given routinely
9. VAGINAL BLEEDING & MENSTRUATION
Vaginal bleeding (known as lochia) will occur for 2 to 6 weeks following delivery. This is the discharge of blood, mucus and tissue from the uterus. The flow is bright red, heavy and may contain clots at first, kind of like having a period at first. It then turns pink to brown and decreases in amount. Use sanitary pads and not tampons. The extra padding of the thicker maternity pads might make sitting more comfortable. If you do not nurse your baby, you can expect to menstruate again within 4 to 8 weeks. The first menstrual flow tends to be heavy and contains clots; it may start, stop, and start again. The second period should be more or less normal. If you are fully breastfeeding, you will not have your period for several months.
10. EXERCISE & BACK CARE
There will be abdominal wall and muscles laxity. Discuss postnatal exercises with the ward staffs prior to your discharge. A good way to tighten and tone muscles is to hold your stomach in. Practice pulling it in while you take sever¬al natural breaths; then relax. Repeat this throughout the day and make it a permanent habit. Women who had caesarean deliveries should wait at least two weeks before exercising.
Pelvic floor muscles support your uterus, bladder, small intestine, and rectum. Pregnancy and difficult vaginal delivery may weaken these muscles, giving rise to urinary leakage and prolapse of pelvic organs (descent of the rectum, vagina, and uterus) in later life. Pelvic floor exercises (also called Kegel exercises) aim to strengthen your pelvic floor muscles. The simplest way to locate your pelvic floor muscles is to stop the flow of your urine in midstream. If you can do it, it means that you are able to contract the specific pelvic floor muscles to stop your urine flow. When you relax, your urine flow should resume. Repeat it again. You should be able to do it easily. Later when the vaginal wound has healed, you can insert a finger in your vagina and try to tighten the muscles around your finger. If you are doing it correctly, your finger will feel the squeeze.
To start off, do the Kegels exercises during urination. Try to squeeze the muscles for ten seconds and then release. Do it several times at each session until you are confident of contracting the correct muscles. Later on, you should continue to do it outside of the toilet, such as while you are sitting, standing, or lying down or when you are performing a task like breastfeeding, cooking, back to work, driving, etc. Squeeze five to ten times per session and try to do three to four sessions a day.
11. ABDOMINAL BINDER
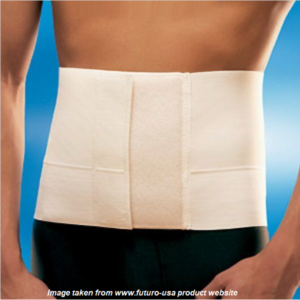 An abdominal binder is broad compression belt that encircles your abdomen. It is usually made from elastic and nylon materials with Velcro, hoop or loop closures. It comes in various shapes, sizes and softness of materials. You may want to wear one after your Caesarean section. It may help to reduce post-operative pain and helps you to move around easily. The compression provided by the binder will also reduce the pain when you cough or sneeze. The wearing of abdominal binder may provide some comfort after the vaginal delivery as well, especially if you have a pendulous abdomen (hanging belly). The pendulous abdomen is due to the distention and overstretching of the abdomen leading to weakened muscles in some women throughout pregnancy and during the pushing at vaginal delivery. Do take note that some women do not find it useful. You should try it if you think there is a need for you. In the end, you may or may not like it.
An abdominal binder is broad compression belt that encircles your abdomen. It is usually made from elastic and nylon materials with Velcro, hoop or loop closures. It comes in various shapes, sizes and softness of materials. You may want to wear one after your Caesarean section. It may help to reduce post-operative pain and helps you to move around easily. The compression provided by the binder will also reduce the pain when you cough or sneeze. The wearing of abdominal binder may provide some comfort after the vaginal delivery as well, especially if you have a pendulous abdomen (hanging belly). The pendulous abdomen is due to the distention and overstretching of the abdomen leading to weakened muscles in some women throughout pregnancy and during the pushing at vaginal delivery. Do take note that some women do not find it useful. You should try it if you think there is a need for you. In the end, you may or may not like it.
So far, there is no scientific evidence to proof that the use of abdominal binder (either after vaginal or caesarean delivery) will get you back in shape faster or helps you to reduce belly fat or your overall weight. It is basically used to reduce pain and provide some comfort. When choosing an abdominal binder, it is important to get the right size and wear it properly. Do make sure it is not too tight and you are able to breath and sit comfortably.
12. MEDICATIONS, SUPPLEMENTS AND IMMUNISATION
 Pain relief medication and a mild laxative is usually prescribed upon discharge. You should continue taking your multivitamins (which should contain iron and folic acid) daily for one to two months. If you are breastfeeding, continue taking your calcium and vitamin D supplements indefinitely until you stop breastfeeding. There is no need to take other supplements. A normal and balanced diet is the best way to ensure optimal health during the recovery and breastfeeding period. Many of the traditional herbal remedies are of unproven values and some (such as ginseng, ginkgo, dong quai) may cause blood thinning leading to excessive uterine bleeding. Furthermore, many preparations do not contain ingredients list and are not manufactured or prepared according to the strict guidelines. Therefore, these are potentially harmful to you and your baby.
Pain relief medication and a mild laxative is usually prescribed upon discharge. You should continue taking your multivitamins (which should contain iron and folic acid) daily for one to two months. If you are breastfeeding, continue taking your calcium and vitamin D supplements indefinitely until you stop breastfeeding. There is no need to take other supplements. A normal and balanced diet is the best way to ensure optimal health during the recovery and breastfeeding period. Many of the traditional herbal remedies are of unproven values and some (such as ginseng, ginkgo, dong quai) may cause blood thinning leading to excessive uterine bleeding. Furthermore, many preparations do not contain ingredients list and are not manufactured or prepared according to the strict guidelines. Therefore, these are potentially harmful to you and your baby.
If you are still not immunized against Rubella or Hepatitis B, you can request the vaccination prior to discharge.
 13. SEXUAL INTERCOURSE
13. SEXUAL INTERCOURSE
In general, sexual intercourse can be resumed after the fourth week postpartum, provided the bleeding has stopped and the perineum (area between the vagina and rectum) is comfortable for the woman. Many women report a low or absent sexual desire during the first few weeks after delivery. Reasons may involve fatigue, weakness, pain with intercourse, vaginal discharge or concern about injury. Discuss this issue with your spouse if you have problems. Most couples resume sexual intercourse by 6 to 8 weeks after delivery. Sexual intercourse can cause some discomfort for the woman because of vaginal dryness (especially in breast-feeding women). Using a water-based gel lubricant (e.g., KY Jelly) may help.
14. CONTRACEPTION
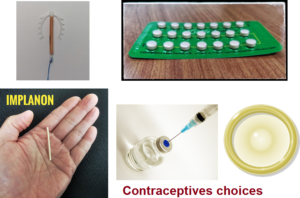 You should discuss this with your doctor. You do not need additional protection if you are fully breastfeeding (no supplementation with infant formula at all). However, it will not be reliable once infant formula is introduced or weaning takes place. If you are providing mixed feeding to your baby, have your partner use a condom until another type of birth control is selected.
You should discuss this with your doctor. You do not need additional protection if you are fully breastfeeding (no supplementation with infant formula at all). However, it will not be reliable once infant formula is introduced or weaning takes place. If you are providing mixed feeding to your baby, have your partner use a condom until another type of birth control is selected.
The choice of hormonal methods of contraception will depends on whether the woman is breastfeeding or not. Contraceptives that contain oestrogen are not suitable for breastfeeding mothers. You should discuss your needs and preferences with your doctor. The intrauterine device, hormonal implants or injections can usually be initiated at the 6-week postpartum check-up.
15. HAIR LOSS
 Some women may encounter excessive hair loss. This shedding is normal. It is due to the hormonal changes during pregnancy and after delivery. Higher oestrogen levels during pregnancy increases promote hair growth and reduce hair loss. Following delivery where there will be an abrupt decline of oestrogen level, this will result in more than the usual amount of hair shedding. It is only temporary, and your hair growth should be back to normal after 6 to 9 months.
Some women may encounter excessive hair loss. This shedding is normal. It is due to the hormonal changes during pregnancy and after delivery. Higher oestrogen levels during pregnancy increases promote hair growth and reduce hair loss. Following delivery where there will be an abrupt decline of oestrogen level, this will result in more than the usual amount of hair shedding. It is only temporary, and your hair growth should be back to normal after 6 to 9 months.
16. THE POSTNATAL “BLUES”
 For some women, the first few weeks at home seems to be quite different and not what is expected. They may have adjustment problems and appeared depressed. Everyone expects the woman to be happy, but she is not. This may be aggravated by fatigue, lack of sleep and sometimes lack of support from family members and friends. Taking care of a newborn for the first few weeks can be a demanding task, especially for the first time mother. She may have increasing doubts about her ability to cope with the 24-hour-a-day demands of mothering. Some women may be weepy and withdrawn. All these changes are due to the adjustment of the body to the sudden drop in the female hormones following delivery. Therefore, it is not uncommon for many women to feel this way. Luckily, this is self-limiting and will often resolve completely within a few weeks. Full support from the husband, family members and friends will help in minimizing the severity and hasten recovery. For some women, professional help may be required if the problem persists or worsens.
For some women, the first few weeks at home seems to be quite different and not what is expected. They may have adjustment problems and appeared depressed. Everyone expects the woman to be happy, but she is not. This may be aggravated by fatigue, lack of sleep and sometimes lack of support from family members and friends. Taking care of a newborn for the first few weeks can be a demanding task, especially for the first time mother. She may have increasing doubts about her ability to cope with the 24-hour-a-day demands of mothering. Some women may be weepy and withdrawn. All these changes are due to the adjustment of the body to the sudden drop in the female hormones following delivery. Therefore, it is not uncommon for many women to feel this way. Luckily, this is self-limiting and will often resolve completely within a few weeks. Full support from the husband, family members and friends will help in minimizing the severity and hasten recovery. For some women, professional help may be required if the problem persists or worsens.
FIRST POSTNATAL VISIT
 The first visit is usually at 6 weeks after delivery. However, you may be asked to come back for review much earlier if there are complications during the antenatal, delivery or postnatal period. During the 6 weeks visit, you will be asked about your general health, vaginal bleeding and any problem with breast-feeding. A physical examination will be performed, including a cervical cancer screening (Thin Prep test) if it is due or never been done before. Contraceptive choices should be discussed and chose the type that is acceptable to you and your partner.
The first visit is usually at 6 weeks after delivery. However, you may be asked to come back for review much earlier if there are complications during the antenatal, delivery or postnatal period. During the 6 weeks visit, you will be asked about your general health, vaginal bleeding and any problem with breast-feeding. A physical examination will be performed, including a cervical cancer screening (Thin Prep test) if it is due or never been done before. Contraceptive choices should be discussed and chose the type that is acceptable to you and your partner.
.
To print a pdf copy of this article, CLICK HERE.