Postmenopausal bleeding is defined as unexpected vaginal bleeding that occurs during the menopausal years. Menopause is the permanent cessation of menstruation and is normally diagnosed after 1 year of absent menstrual flow.
Postmenopausal bleeding is defined as unexpected vaginal bleeding that occurs during the menopausal years. Menopause is the permanent cessation of menstruation and is normally diagnosed after 1 year of absent menstrual flow.
Symptoms and signs
- Vaginal bleeding, which may be a light-brown discharge or heavy, red bleeding (with or without clots). Mucus may accompany the bleeding. Bleeding episodes may vary in length.
- Women who are on hormonal replacement therapy may have some bleeding and this can be normal, depending on the type of hormone that she is taking. Please consult your doctor about the types of bleeding to be concerned about.
- Presence of excessive bleeding, progressive abdominal distention, pain and feeling
unwell usually signify a more serious problem.
Causes
- Endometrial or vaginal atrophy (shrinking or wasting away of tissue which line the reproductive tract).

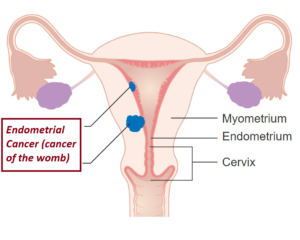
- Cancer of the reproductive system (up to 10% of the cases of post menopausal bleeding are due to cancer).
- Irritation or infection of the membranes lining the uterus, vagina and vulva.
- Injury or trauma to the vagina, associated with reduced oestrogen levels.
- Polyps or benign tumours of the cervix.
- Polyps on the inner uterine lining (endometrial polyps); fibroids.
- Hormone therapy that stimulates the endometrium (uterine lining), causing sloughing
similar to normal menstruation. Oestrogens (female hormones) used irregularly are a
common cause of this. - Disorders of the blood cells, lymphatic system or bone marrow, causing problem with
clotting. - Liver disorders.
- Medications – anticoagulant or aspirin-containing drugs.
Complications
- Anemia.
- If cancer is the cause, it may spread to other body parts.
Investigations and diagnosis
- Laboratory blood studies – Haemoglobin, clotting studies, tumour markers.
- Pap smear (cervical cancer screening – cytology).
- Ultrasound scan of the reproductive organs.
- Evaluation of the uterine cavity via either:
- Diagnostic hysteroscopic (telescopic instrument with fiber-optic light) examination. Any abnormal area in the cavity can be taken for further examination (biopsy) to exclude cancer. At the same time, endometrial polyps and small fibroids can be removed with specialized instruments.

- Saline infusion sonohysterography (SIS) (ultrasound with a salt-water solution injected into the uterus).
- Biopsy of the endometrium, using a small disposable catheter. This can be performed in the clinic, with minimal discomfort. This commonly done now, instead of the formal dilatation and curettage (referred to as D & C, which is dilatation of the cervix and a scraping out of the uterus with a curette).
Sometimes, even after the testing, no clear-cut reason for the bleeding is found.
 Treatment
Treatment
- Specific therapy is dependent on the cause.
- The most common cause of postmenopausal bleeding is an atrophic endometrium.
- This often does not need treatment. If the problem persists, hormone replacement therapy may be given.
- If hormone replacement medications are currently being taken, the dose may need to be adjusted.

- Vaginal moisturizer is helpful in women with thinning of the vagina wall.
- Endometrial polyps should be removed using the hysteroscope to exclude cancer.
- Surgery (hysterectomy) to remove the uterus may be needed in certain circumstances.
- Resume your normal activities as soon as symptoms improve.
- Sexual relations may be resumed as soon as desired after diagnosis and treatment.
See your doctor if there is:
- Bleeding recurred again after evaluation or following treatment.
- Increasing bleeding which soaks more than 1 pad or tampons each hour.
- Persistent and abnormal vaginal discharge.
- Signs of infection such as headache, muscle aches, dizziness or a general ill feeling
and fever.
To print a pdf copy, click HERE
[mailerlite_form form_id=3]