Heartburn is a term used to describe a burning pain or discomfort in the chest and upper abdomen. The actual medical term for it is gastro-esophageal reflux disease (GERD). It is quite common for pregnant women to experience the symptoms of heartburn, which usually come and go until delivery. It can start anytime during the pregnancy period and may worsen as the pregnancy progresses (second or third trimester). While it can be uncomfortable or painful, heartburn by itself will not harm the baby.
Heartburn is a term used to describe a burning pain or discomfort in the chest and upper abdomen. The actual medical term for it is gastro-esophageal reflux disease (GERD). It is quite common for pregnant women to experience the symptoms of heartburn, which usually come and go until delivery. It can start anytime during the pregnancy period and may worsen as the pregnancy progresses (second or third trimester). While it can be uncomfortable or painful, heartburn by itself will not harm the baby.
Symptoms and signs
- Burning pain in the center of the chest and the upper abdomen, frequently accompanied by an unpleasant taste in the mouth.
- Belching (burping).
- Nausea with or without vomiting.
- Persistent throat irritation, with or without irritating dry cough.
Sometimes, symptoms may be worse in the middle of the night and upon waking up in the morning
Causes
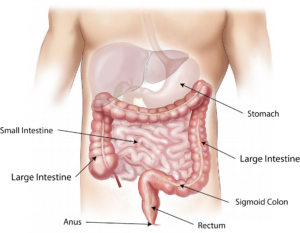 Heartburn is not associated with a heart disorder. It is due to a backflow of acid from the stomach into the esophagus. The muscles that close off the upper part of stomach into the esophagus become lax, thus allowing the stomach acid juices to enter the esophagus and irritate its lining. The laxity of the muscles is due to a pregnancy hormone called progesterone. During pregnancy, there are several changes in the gastrointestinal functions which lead to an increase in stomach acid production and a slower emptying time of the stomach contents. As pregnancy advances, the enlarged womb presses on the stomach and increase the pressure on it. All these changes during pregnancy contributed to the onset of heartburn symptoms.
Heartburn is not associated with a heart disorder. It is due to a backflow of acid from the stomach into the esophagus. The muscles that close off the upper part of stomach into the esophagus become lax, thus allowing the stomach acid juices to enter the esophagus and irritate its lining. The laxity of the muscles is due to a pregnancy hormone called progesterone. During pregnancy, there are several changes in the gastrointestinal functions which lead to an increase in stomach acid production and a slower emptying time of the stomach contents. As pregnancy advances, the enlarged womb presses on the stomach and increase the pressure on it. All these changes during pregnancy contributed to the onset of heartburn symptoms.
Risk factors
- Overeating or eating and then lying down immediately.
- Prior history of gastric disorders such as peptic ulcer disease or gastro-esophageal reflux.
- Obesity
Certain activities or food intake can aggravate it – smoking, eat close to bedtime, eat fatty, spicy or fried foods, drink caffeine beverages, drink alcohol, use of nonsteroidal anti-inflammatory drugs (NSAIDs) like aspirin or mefenamic acid.
Prevention
Avoid the risk factors listed above.
Expected outcomes
This can be uncomfortable but usually does not lead to significant complications to you and your baby. It will improve after delivery in the majority of women unless the cause is not related to pregnancy.
Complications
- Heartburn can affect your ability to eat a healthy diet, leading to poor weight gain.
- Progressive worsening may lead to esophageal ulcers and an increased risk of bleeding.
 Treatment
Treatment
- Diagnosis is usually made from the history and the risk factors present. Invasive tests are unnecessary during pregnancy.
- Simple lifestyle changes must be made first to lessen the symptoms.
- Avoid bending over, especially after eating or while doing abdominal exercises.
- Avoid eating while lying down.
- Do not wear tight girdles or belts.
- Place books or blocks under the head of your bed to raise it about 10 cm or more, or sleep propped up with several pillows.
- Dietary changes (see below).
- In many instances, symptoms may improve without medications. Or if symptoms are mild and you can live with it, medication is usually not necessary. However, in some cases, it may be of benefit. Simple antacid liquid mixtures or tablets are usually the first choice and may be helpful. These drugs should be used only with your doctor’s recommendation. Other stronger medications (the proton-pump inhibitors such as omeprazole) may be prescribed if the above measures do not work.
- Avoid taking any herbal supplements without asking your doctor.
- Stay active.
- Look out for certain trigger foods that can trigger your heartburn symptoms.
 Dietary advise
Dietary advise
- Eat small, frequent meals.
- Do not rush through your meals, learn to eat slowly.
- Avoid drinking large quantities of fluids during meals.
- Do not eat before bedtime.
- Avoid highly seasoned food or spicy food.
- Avoid caffeine beverages.
- Avoid citrus foods/drinks and tomatoes.
- Do not drink alcohol or smoke
See your doctor immediately if there is:
- Medications do not bring relief.
- Vomiting late in pregnancy.
- The vomit material that has blood in it or looks like coffee grounds.
- Your stools colour changes to black or tarry stools. These may suggest bleeding in the stomach and need urgent medical treatment
To download a pdf copy, click HERE
To subscribe, click HERE