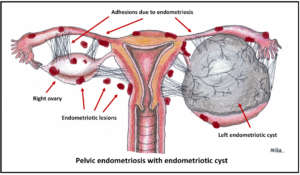
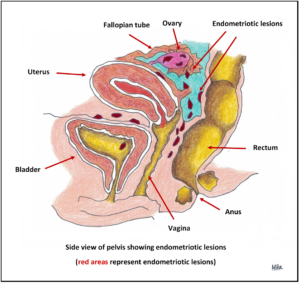
 Endometriosis is a condition whereby tissues from the lining (endometrium) of the uterus becomes implanted in areas outside the uterus such as the outer surface of the uterus, the fallopian tubes or the ovaries. Rarely, the endometrial tissue may spread beyond the reproductive organs and pelvic region.
Endometriosis is a condition whereby tissues from the lining (endometrium) of the uterus becomes implanted in areas outside the uterus such as the outer surface of the uterus, the fallopian tubes or the ovaries. Rarely, the endometrial tissue may spread beyond the reproductive organs and pelvic region.
In a normal menstrual cycle, the endometrial tissues respond to cyclical female hormones and becomes progressively thicker and will eventually shed each month if the woman is not pregnant. It is discharged as menstrual flow at the end of each cycle. In endometriosis, this shedding and bleeding will occur outside the uterus as well, causing significant pain. Recurrent bleeding and healing cycle will eventually cause scar tissue formation and destruction of pelvic structures. The excessive blood will accumulate over a period of time and eventually forms a cyst in the ovary (called endometriotic cyst or endometrioma). The 4 stages (classification) of endometriosis (minimal, mild, moderate or severe) are used to describe the location and the severity of the disorder.
Incidence
 Endometriosis can affect females between puberty and menopause but is most common between ages 20 and 35. Endometriosis is estimated to affect approximately up to 10% of reproductive aged women.
Endometriosis can affect females between puberty and menopause but is most common between ages 20 and 35. Endometriosis is estimated to affect approximately up to 10% of reproductive aged women.
Causes
The cause is not known. Research is still ongoing to pinpoint the cause. The pre-dominant theory is that during menstruation, some of the menstrual tissue (endometrium) backs up through the fallopian tubes into the pelvis (retrograde menstruation), where it implants and grows. Another theory is that endometriosis may be a genetic process, or that certain families may have predisposing factors to endometriosis. It is still unclear whether there is an environmental or external trigger that starts off the disease process in those susceptible women.
Risk factors
- Early onset of menses and increasing age
- Women who do not become pregnant or who delay childbirth
- Women with family history of endometriosis
- Abnormalities of the internal genital organs (either the uterus, tubes, cervix or vagina) that interfere with the monthly menstrual flow
Symptoms and signs
Endometriosis can present in many ways in different women. A significant number of women do not have symptoms at all. Some may present with severe and debilitating pain. When you have your period, the misplaced endometrial tissue swells and bleeds, just like the lining of your uterus. The following symptoms may begin abruptly or develop over many years:
- Increased pelvic pain during menstrual periods
- Pain with sexual intercourse.
- Lower abdominal pain, can be in midline or on either side, even when not menstruating
- Premenstrual spotting.
- Back pain, which can be localized to the sacral area. Sometimes the pain can radiate to the posterior upper thigh
- Pain with intestinal contractions, bloating and possible change of bowel habits. It may mimic irritable bowel syndrome (IBS) or may make it worst
- Difficulty in getting pregnant
- Blood in the stool (sometimes) or painful defecation during menses.
- Urinary symptoms – such as painful urination, frequency, blood in the urine.
- Rare symptoms – perimenstrual chest, shoulder or abdominal wall pain,
Complications
- Infertility (from implants that cause adhesions or scar tissue and cause tubal blockage).
- Rupture of the endometriotic cyst causing pain
- Infection of the endometriotic cyst
- Causing obstruction to the ureter (a tube that channel urinary flow from the kidney to the bladder) and bowels
- Chronic pelvic pain that causes stress and disruptions in lifestyle.
- Adhesions of pelvic organs.
- Implants on the ovary can lead to large cysts and pelvic masses called endometrioma or endometriotic cyst.
Diagnosis
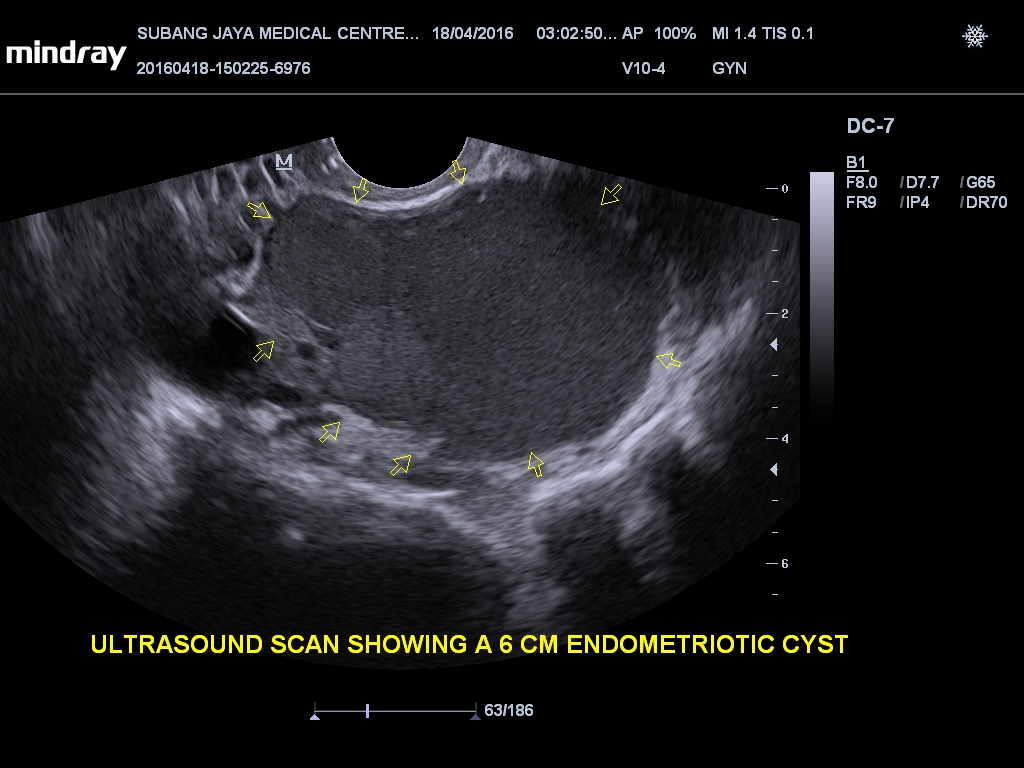
 Diagnosing the disorder is usually accomplished with a laparoscopy procedure. A laparoscope (telescopic instrument with fiber optic light) is inserted into the abdomen through a small incision, and visual examination of abdominal and pelvic organs is possible. This method is the most accurate assessment of sites and severity of the disease. Ultrasound scan of the pelvis is only useful for the diagnosis of endometriotic cyst. It will not be able to diagnose mild endometriosis without the presence of a cyst in the ovary. Magnetic Resonance Imaging (MRI) may be done if the ultrasound scan is inconclusive and to look endometriotic lesions between the uterus and the rectum.
Diagnosing the disorder is usually accomplished with a laparoscopy procedure. A laparoscope (telescopic instrument with fiber optic light) is inserted into the abdomen through a small incision, and visual examination of abdominal and pelvic organs is possible. This method is the most accurate assessment of sites and severity of the disease. Ultrasound scan of the pelvis is only useful for the diagnosis of endometriotic cyst. It will not be able to diagnose mild endometriosis without the presence of a cyst in the ovary. Magnetic Resonance Imaging (MRI) may be done if the ultrasound scan is inconclusive and to look endometriotic lesions between the uterus and the rectum.
The blood test CA-125 has been shown to be elevated in patients with severe endometriosis but its usefulness is limited in diagnosing endometriosis. It is not routinely done.
Treatment
- Without treatment, endometriosis will become increasingly more severe. It subsides after menopause when oestrogen production decreases or ceases.

- Symptoms can be relieved with medication, and/or surgery. The type of treatment will vary, depending on the stage of the disease, symptoms, the patient’s age, and desire to have children.
- Pain symptom can be relieved with nonsteroidal anti-inflammatory drugs (NSAIDs). If the pain is severe during menstruation, the pain medication should be started as soon as the menstrual flow begins (e.g. on the first day). Do not wait until the day of maximal pain before starting the painkillers. By then, it is too late and often not effective.
- Combined oral contraceptive pills is a good choice if there is associated heavy menstrual flow and there is a need for contraception. It can be taken cyclically or continuously for several packs. The commonest types of pills comes in a 21 days pack (with all the pills containing the same oestrogen and progestogen dosage) and in endometriosis, it is better to take the pills continuously for 2 or 3 packs before a 7 days break (to allow withdrawal menstrual shedding) so that there will be less menstrual cycles in a year.

- Progestogens – this is a synthetic hormone that induces thinning and atrophy of the endometrial tissue and reduces menstrual flow. It can be given orally or as an injection every 3 months (marketed as Depo-Provera). The oral progestogens is to be taken daily and the available formulations are: norethisterone, dienogest (Visanne), medroxyprogesterone acetate, dydrogesterone. The most commonly use progestogen for endometriosis is dienogest. The side-effects most commonly seen with progestogen usage include troublesome breakthrough uterine bleeding, weight gain, abdominal bloating, oedema, acne and mood changes.
- Gonadotropin-releasing hormones (GnRH) injection work by suppressing ovarian function. It will induce a state of pseudo-menopause and can only be use for 6 months because of bone demineralization (osteoporosis). Side effects are similar to peri-menopausal symptoms and is only transient – hot flushes, sweating, palpitations, mood changes. It is reserved for those with significant pain symptoms following surgery. You may have menstrual bleeding 1 to 2 weeks after the first injection. Following this, you will not have menses during subsequent injections.
- If you want children, consider pregnancy as soon as possible. Pregnancy may offer some relief from the disorder. Delaying pregnancy may result in infertility.
- Surgery – this is necessary if
- has symptoms due to endometriosis and medication did not work
- presence of endometriotic cyst.
- ruptured endometriotic cyst with persistent pain symptoms
- desire for pregnancy when there is suspicion that the infertility may be due to endometriosis.
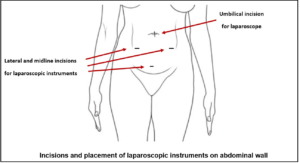 The type of surgery will depend on several factors such as age of the woman, her symptoms, number of previous surgeries, sites of disease, severity and desire for pregnancy. Laparoscopic surgery is the method of choice. Sometimes this is not feasible and open surgery will be required. Surgical options include removal of endometriotic cyst (called cystectomy), removal of one or both ovaries, destruction or excision of lesions of endometriosis and restoring the pelvic organs anatomy. In those with recurrence and who had completed family, an operation to remove the uterus (hysterectomy), fallopian tubes and both ovaries may be necessary to deal with this problem. This will result in menopause and is considered a cure for endometriosis. Following this, hormone replacement therapy can be given for those who are in the premature menopause group or developed significant menopausal symptoms.
The type of surgery will depend on several factors such as age of the woman, her symptoms, number of previous surgeries, sites of disease, severity and desire for pregnancy. Laparoscopic surgery is the method of choice. Sometimes this is not feasible and open surgery will be required. Surgical options include removal of endometriotic cyst (called cystectomy), removal of one or both ovaries, destruction or excision of lesions of endometriosis and restoring the pelvic organs anatomy. In those with recurrence and who had completed family, an operation to remove the uterus (hysterectomy), fallopian tubes and both ovaries may be necessary to deal with this problem. This will result in menopause and is considered a cure for endometriosis. Following this, hormone replacement therapy can be given for those who are in the premature menopause group or developed significant menopausal symptoms.
Recurrence
Endometriosis can recur, even after surgery. The risk of recurrence is higher is those with severe disease and reported to be in the range of 20 to 30%.
To download and print a pdf copy, CLICK HERE
To view animation on endometriotic cyst, CLICK HERE
To read more about laparoscopic surgery, CLICK HERE
To view videos of laparoscopic surgery for endometriosis, CLICK HERE
Please subscribe HERE to receive the regular newsletter and get the latest updates regarding Women’s Health