Dr. William Morton demonstrated the first public administration of ether anaesthesia in the operating theatre of the Massachusetts General Hospital on the 16th October 1846
Dr. William Morton demonstrated the first public administration of ether anaesthesia in the operating theatre of the Massachusetts General Hospital on the 16th October 1846
That day is remembered as a milestone in anaesthesia and celebrated as World Anaesthesia Day.
From that date onward, many progresses have been made in the field of anaesthesia, and more so specifically for the practice of obstetrics and gynaecology.
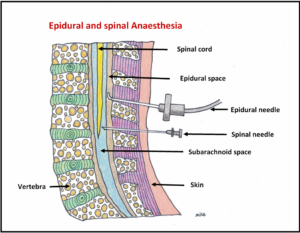
On the 16th August 1897, a German surgeon by the name of Dr. August Bier administered the first spinal anaesthetic. 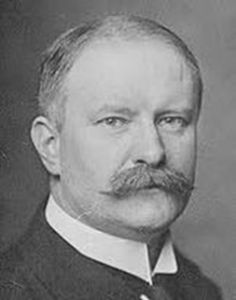 Spinal anaesthesia becomes one of the most popular methods of administering a patient pain free from surgery of the lower limbs, lower abdomen and Caesarean sections and is still widely used.
Spinal anaesthesia becomes one of the most popular methods of administering a patient pain free from surgery of the lower limbs, lower abdomen and Caesarean sections and is still widely used.
In 1945, the Tuohy epidural needle is introduced into clinical practice and is widely used to produce epidural analgesia which is another common method of pain relief used for mothers in labour.
Types of anaesthesia
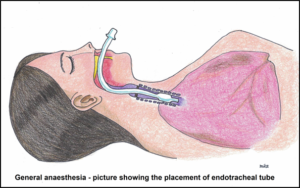
- General Anaesthesia – general anesthesia or commonly known as GA is the state produced when a patient receives medications to lose consciousness, receive pain relief and muscle paralysis to allow surgery to be performed.
 General anesthesia uses a combination of intravenous and inhaled anaesthetics agents to allow adequate surgical access to the operative site.
General anesthesia uses a combination of intravenous and inhaled anaesthetics agents to allow adequate surgical access to the operative site. - Spinal & Epidural Anaesthesia – spinal and epidural anaesthesia are types of anaesthesia is which a local anaesthetic is injected near the spinal cord, specifically the lumbar nerve root of the body which is at the lower back of your body above the buttocks. Spinal anaesthesia are used primarily for surgery of the lower abdomen and the legs, as such making it suitable for Caesarean section.
 Epidurals are now one of the more popular methods of pain relief during labour. Most people will experience a warm, tingling sensation as the anaesthetic medication numbs the nerve. This is followed by complete numbness usually lasting between 1 and 4 hours before it starts to disappear, and you will begin to feel sensation and can move your legs. For epidural, the effect is much more gradual and will last for as long as the catheter is in place and medicines are being infused via the catheter. Both methods may have side effects such as nausea or vomiting, headache, giddiness and are expected to last a few hours. Very rarely these effects may last longer, and your doctor will advise what needs to be done. You must rest in bed until the numbness goes away.
Epidurals are now one of the more popular methods of pain relief during labour. Most people will experience a warm, tingling sensation as the anaesthetic medication numbs the nerve. This is followed by complete numbness usually lasting between 1 and 4 hours before it starts to disappear, and you will begin to feel sensation and can move your legs. For epidural, the effect is much more gradual and will last for as long as the catheter is in place and medicines are being infused via the catheter. Both methods may have side effects such as nausea or vomiting, headache, giddiness and are expected to last a few hours. Very rarely these effects may last longer, and your doctor will advise what needs to be done. You must rest in bed until the numbness goes away. - Peripheral Nerve Blocks – these are types of anaesthesia that uses local anaesthesia medication to numb specific nerve roots and trunks on your limbs, abdomen or chest so that only areas innervated by the nerves are blocked and no pain will be felt.

- Sedation – This are usually given for procedures that are not very painful and short such as gastroscopy, small excision of lumps and sometimes dental procedures. They can be given orally, via injections as well as a light anaesthetic gas such as nitrous oxide.
- Local Anaesthetics – this involves injection of local anaesthesia medications to the skin and subcutaneous tissues such as during dental procedures or minor skin surgery so only that area that has been infiltrated with the solutions is rendered pain free.
Risk of Anaesthesia
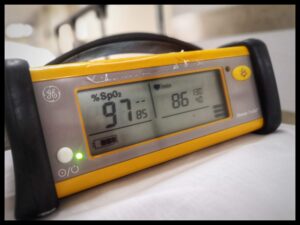
 With modern advances in medications, monitoring technology, and safety systems, as well as highly educated anaesthesia providers, the risk caused by anaesthesia to a patient undergoing routine surgery is small. Mortality attributable to anaesthesia is said to occur at rates of less than 1:100,000. However small the risk is, patients will still need to be aware of some of the common effects and risks associated with all anaesthesia techniques.
With modern advances in medications, monitoring technology, and safety systems, as well as highly educated anaesthesia providers, the risk caused by anaesthesia to a patient undergoing routine surgery is small. Mortality attributable to anaesthesia is said to occur at rates of less than 1:100,000. However small the risk is, patients will still need to be aware of some of the common effects and risks associated with all anaesthesia techniques.
Preparation
Before having an operation, you will be meeting your anaesthetist and planning your anaesthetic together. Your anaesthetist will look at your medical history and will ask whether anyone in your family has had problems with anaesthesia. They will also ask about your general health and lifestyle, including whether you have allergies or taking any other medication.  Please inform your healthcare provider or anaesthetist if you are currently still taking any herbal supplements. This is important because some herbs or supplements can cause bleeding or interact with anaesthetic drugs. Your anaesthetist will also be able to answer any questions you have. Let them know if you are unsure about any part of the procedure or if you have any worries or concerns.
Please inform your healthcare provider or anaesthetist if you are currently still taking any herbal supplements. This is important because some herbs or supplements can cause bleeding or interact with anaesthetic drugs. Your anaesthetist will also be able to answer any questions you have. Let them know if you are unsure about any part of the procedure or if you have any worries or concerns.
You will be given clear instructions to follow before the operation, including whether you can eat anything in the hours leading up to it. Normally you should be fasted for at least 6 hours to allow time for your stomach to have minimal content. You will also be given some prophylactic medications to reduce the stomach acidity in the event you may need GA for the Caesarean Section. You will also need to inform the anaesthetist if you have dentures, crowns or bridges so that the anaesthetist will be aware in the event a tube has to be inserted via the oral cavity into your windpipe. Dentures need to be removed while permanently fixed crown or bridges can stay in place as it is. After the surgery is over, common things that will occur include drowsiness, nausea, vomiting, sore throat, dry mouth, dry lips as well as sore throat if the surgery was done under GA. Inability to pass urine may occur after a spinal or epidural anaesthesia and sometimes a urinary catheter is inserted while waiting for normal function of the bladder to return. Most of these symptoms settles after a day or two at most after surgery. These are usually mild and settles with some medication.
Most patient are also concerned with management of pain after surgery. This can be discussed with the anaesthetist and suitable options include regular injections of analgesics, patient controlled analgesia using a machine that can deliver medications on demand by the patient as well as continuation of the epidural analgesia for a day or two after the surgery is over.
Pain relief for labour and delivery
 This subject has been extensively studied over the years and has made the experience of labour a much more pleasant one. Contraction pains can be stressful and lead to increased stress responses as manifested by high blood pressure and rapid pulse rate. For some mothers with underlying medical conditions like hypertension, heart disease and anxiety disorder, these changes can be quite detrimental. The various options for pain relief are:
This subject has been extensively studied over the years and has made the experience of labour a much more pleasant one. Contraction pains can be stressful and lead to increased stress responses as manifested by high blood pressure and rapid pulse rate. For some mothers with underlying medical conditions like hypertension, heart disease and anxiety disorder, these changes can be quite detrimental. The various options for pain relief are:
- Injection of medications – most of these medications are opioid based such as morphine and pethidine.
 Generally, they are given at the early stages of your labour pain. The side effects associated with this include nausea and vomiting. If given at very regular doses or a dose has been given just before your baby is delivered, there is a small risk that your baby will be over sedated after delivery and require an antidote to reverse the effects of the opioids.
Generally, they are given at the early stages of your labour pain. The side effects associated with this include nausea and vomiting. If given at very regular doses or a dose has been given just before your baby is delivered, there is a small risk that your baby will be over sedated after delivery and require an antidote to reverse the effects of the opioids. - Inhalational agents – a combination of nitrous oxide and oxygen at 1 :1 ratio allows some form of analgesic relief for labour pain. It is also quick to administer and the easy to use. This type of pain relief if only suitable towards the end of labour when delivery is imminent. The side effects are usually mild with some reporting dizziness, and nausea or vomiting. The inhalational agents are generally safe to the baby.
- Epidural – epidural anaesthesia is considered the gold standard for pain relief during labour. You can request your obstetrician to refer you to an anaesthetist and he will have a discussion with you on whether you are a suitable candidate for an epidural anaesthesia.
-
- The procedure involves inserting a large needle into the epidural space under local anaesthesia. This is the space between the dura mater (a membrane protecting the spinal cord) and the spinal subarachnoid space. A local anaesthesia is given first to numb the area where the needle is introduced. Upon successful entry into the space that usually is at the lower back region, a thin plastic tubing is inserted into the space and left in place.
- Medications are then administered via this tubing throughout the duration of your labour and you will feel immediate pain relief if the procedure was successful. Occasionally, you may still sense contractions but as long as you are comfortable, the doses can be titrated (either increased or decreased) to give you the best pain relief.
- As the epidural procedure requires significant expertise to perform, your anaesthetist will inform you on how its being done before getting your consent. Some common risks include post dural puncture headache (about 1 in 100 patients), epidural infection and bleeding leading to blood clot in the spinal cord (1 in 100,000 to 200,000 patients). Nausea or vomiting are usually mild. Some patients have reported itchiness, and this is attributed to some of the medications that are used in your epidural. Numbness or cramp like sensations can occur too and can be minimized by reducing the infusion rate of your medications. Long term complications like back ache or paralysis are extremely rare.
- Effects to the baby are negligible as these medications do not cross over the placenta in significant amounts.
- Occasionally, if your obstetrician has decided that you need a Caesarean Section, the epidural can be used to render the area of surgery numb as well so that General Anaesthesia can be avoided.
Anaesthesia for Caesarean Section
- General Anaesthesia (GA) – this is rarely used now. It may be indicated when the baby’s or mother’s condition is unstable and requires urgent delivery or when the spinal or epidural placement is contraindicated.
 Sometimes, conversion to GA may occur when the anaesthetist is unable to conduct spinal anaesthesia due to various reasons or the effect of spinal anaesthesia is inadequate to provide total pain free (total block) for the operation. The method of GA is called rapid sequence induction where a few medications are administered to render you unconscious and a tube is inserted into your windpipe before the surgeon begins the operation.Many patients are concerned as well on whether GA is harmful to the fetus.As some of the medications that are given to the mother to render her unconscious can cross over to the baby via the placental circulation, the risk of the baby becoming drowsy and not breathing well after delivery is a possibility.Due to the significant potential issues of GA during Caesarean Section, the main mode of anaesthesia nowadays is either via spinal or epidural anaesthesia.
Sometimes, conversion to GA may occur when the anaesthetist is unable to conduct spinal anaesthesia due to various reasons or the effect of spinal anaesthesia is inadequate to provide total pain free (total block) for the operation. The method of GA is called rapid sequence induction where a few medications are administered to render you unconscious and a tube is inserted into your windpipe before the surgeon begins the operation.Many patients are concerned as well on whether GA is harmful to the fetus.As some of the medications that are given to the mother to render her unconscious can cross over to the baby via the placental circulation, the risk of the baby becoming drowsy and not breathing well after delivery is a possibility.Due to the significant potential issues of GA during Caesarean Section, the main mode of anaesthesia nowadays is either via spinal or epidural anaesthesia. - Spinal Anaesthesia
Spinal anaesthesia is done using a small needle to inject with medication injected directly into the spinal cord space that contains the cerebrospinal fluids cerebrospinal fluids that surround the spinal cord. The injection is usually made in the lumbar region L2/3 or L3/4 space.
This is now the commonest method of performing anaesthesia for Caesarean Section due to the ease of performing it, the safety aspects of it as well as the advantage of having the mother being awake and breathing on her own. An added advantage is also the possibility of the maternal and child bonding that can be initiated after the delivery itself. - Epidural
Epidural anaesthesia is frequently used to provide pain relief during labour. in fact, it is the most effective pain relief method for labour and delivery. In the event the pregnant mother requires a Caesarean Section for delivery of the baby, the same epidural can be used to top up medications into the epidural space that will allow surgery to be done. This catheter will be removed once the surgery has been completed.
Occasionally, some mothers may feel pain or discomfort during Caesarean Section under epidural anaesthesia. This is usually attributed to the patchiness of the block as some nerve fibres may not be adequately blocked with an epidural compared to spinal anaesthesia. If the pain or discomfort is not bearable, the anaesthesiologist will have to perform GA to allow for the surgery to proceed safely.
Anaesthesia for Gynaecology
- Sedation – minor procedures such as removal of small cysts, dilatation and curettage can be performed with sedation using intravenous or inhalational anaesthetic agents.
- General Anaesthesia (GA) – most gynaecology procedures such as hysterectomy, cystectomy as well as laparoscopic surgery are performed using general anaesthesia. As the patient is generally not in a pregnant state, the performance of GA is a lot more straightforward and very safe. Occasionally, gynaecology procedures are performed in pregnant ladies. For procedures done when the mother is at less than 12 weeks, a small risk of miscarriage is a possibility. Effects to the fetus from the GA after the first trimester (12 weeks and above) is usually minimal and generally safe.
Article written by Dr Gunalan Palari (Consultant Anaesthetist)
Subang Jaya Medical Centre
To download a pdf copy of this article, CLICK HERE