WHAT IS IT?
 Delivery of a baby through an incision in the mother’s lower abdominal and uterine walls and is performed when a vaginal delivery is not possible or is unsafe. This procedure is also called a C-section or Lower Segment Caesarean Section (LSCS).
Delivery of a baby through an incision in the mother’s lower abdominal and uterine walls and is performed when a vaginal delivery is not possible or is unsafe. This procedure is also called a C-section or Lower Segment Caesarean Section (LSCS).
REASONS FOR PROCEDURE
 Danger to the mother or baby from one or more of many causes, including:
Danger to the mother or baby from one or more of many causes, including:
- Baby’s head too large to pass through the birth canal.
- Baby in the wrong orientation – head up (breech) or transverse.
- Failure of cervix to dilate (failed induction of labour).
- Abnormal placenta location obstructing the birth canal (placenta praevia).
- Failure of normal labour progress.
- Situation where urgent delivery is indicated such as fetal distress or severe illness in the mother (such as severe hypertension or sudden fits).
- Infection such as HIV or acute herpes genitalis infection in the mother.
Special situations: pregnancy resulting from assisted reproductive technology (ART), maternal request
POSSIBLE COMPLICATIONS
- Excessive bleeding or surgical-wound infection.

- Post-operative anaemia
- Endo-myometritis (inflammation of lining and muscle of the uterus).
- Excessive scar formation (called keloid scars).
- Complications of anaesthesia.
- Higher possibility of caesarean section in next pregnancy, depending on how the uterine (not skin) incision was done.
- Blood clots in calf veins, which can travel to the lung, causing lung damage.
- In rare situations, there can be injury to the bladder, intestine or other structures encountered during the surgery.
BEFORE THE OPERATION
- Consent for operation should be signed.

- Relevant investigation that may be taken will depends on your medical illness and age.
- A small enema is given the night before or on the morning of the surgery to empty the bowel.
- Shaving of the operative site is done before surgery.
- You are required to fast for at least 6 hours before surgery (no food or drinks at all for 6 hours). For example, if the surgery is in the morning, you should skip breakfast. If it is in the afternoon, you can have an early light breakfast (eg. tea/coffee/milo and toast) but make sure that this is taken at least 6 hours before the surgery. Please reconfirm this with your doctor.
- Oral antacids will be given just prior to the surgery.
DESCRIPTION OF PROCEDURE
- A regional or general anesthesia is administered.
- A urinary catheter is placed and usually removed the following day.
- Antibiotics to prevent post surgical infection is usually given during the surgery.
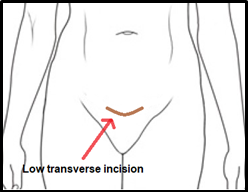
- A transverse incision is made in the lower abdomen (at the level or slightly below the panty line). The incision has to go through several layers – skin, fat, fascia (connective tissue) and finally into your uterus.

- Baby, placenta and birth sac are removed.
- The uterus is closed with absorbable sutures.
- The skin can be closed with either absorbable or non-absorbable sutures. If non absorbable sutures are used, the sutures will be removed in about 1 week after surgery.
- The surgery usually takes 45 to 90 minutes to complete.
POST OPERATIVE CARE
- Expect a hospital stay of 3 to 5 days.
- Fluids will be given via an intravenous line after the surgery to maintain nourishment and hydration.
 Sips of water will be allowed gradually over the first few hours. If you feel well and not nauseous, you will be given nourishing fluids such as a cup of tea/coffee/milo. The drip will be stopped when you are drinking normally again. This may take a little longer if you have had a general anaesthetic. Your doctor will review periodically to decide when to start soft diet.
Sips of water will be allowed gradually over the first few hours. If you feel well and not nauseous, you will be given nourishing fluids such as a cup of tea/coffee/milo. The drip will be stopped when you are drinking normally again. This may take a little longer if you have had a general anaesthetic. Your doctor will review periodically to decide when to start soft diet. - As soon as you begin to feel sensation coming back into your legs, point and flex your feet, circle your ankles and flex at your knees to improve circulation and reduce blood clots in your leg veins.
- Antibiotics may be prescribed for those at risk of infection.
- Pain relief medication should generally be required for only 2 to 7 days following the procedure.
- Pregnancy and caesarean section predispose the woman to a higher risk of deep vein thrombosis and pulmonary embolus. A deep-vein thrombosis (DVT) is a blood clot that develops within a deep vein, most commonly in the leg. Symptoms of a DVT include pain, swelling, and tenderness, usually in the calf, and a rope-like hardness running down the back of the lower leg A pulmonary embolus is a blood clot within the lung, which is often a clot that has dislodged from one of the deep veins of the leg and made its way to the lung. Both conditions are rare. You may be given an injectable medication to reduce your risk of developing deep vein thrombosis and pulmonary embolus. This type of medication is a blood thinning agent, which helps to prevent blood clots. However, side effects will include excessive bleeding from the uterus, wound haematoma and bruising from the injection sites.
 The decision to give is based on various medical guidelines and your risk profiles. It is recommended to be given for 10 days. Other measures to reduce this risk are wearing compression stockings immediately after the Caesarean, ensure adequate hydration, mobilized early (preferable on the following day) and intermittently moving your lower limbs while sitting or lying down. You should continue doing these even when you are at home.
The decision to give is based on various medical guidelines and your risk profiles. It is recommended to be given for 10 days. Other measures to reduce this risk are wearing compression stockings immediately after the Caesarean, ensure adequate hydration, mobilized early (preferable on the following day) and intermittently moving your lower limbs while sitting or lying down. You should continue doing these even when you are at home. - Getting up from bed on the following day – it is easier if you roll to your side at the edge of the bed.
 Put your head on your elbow, then slowly dropping both legs over the side of the bed. At the same time, slowly push yourself up sideways with your elbow and sitting up slowly into a sitting position. Try to use the other hand for support by crossing it over your body. Sit for a while on the bed to get your balance and then slowly stand up. You can do the opposite to get back into bed (in reverse order). By using this method, you will put less pressure on the stitches and abdomen.
Put your head on your elbow, then slowly dropping both legs over the side of the bed. At the same time, slowly push yourself up sideways with your elbow and sitting up slowly into a sitting position. Try to use the other hand for support by crossing it over your body. Sit for a while on the bed to get your balance and then slowly stand up. You can do the opposite to get back into bed (in reverse order). By using this method, you will put less pressure on the stitches and abdomen. - Frequent uterine cramps will be present and will respond to simple pain relief medications.
Gas pain (abdominal wind) can be a problem following the operation for some women. Early mobilization will help to reduce the wind. If the problem still persists, medication can be prescribed for relief. - There will be fresh vaginal bleeding for 1 to 2 weeks and will usually reduce in amount and change in colour with time. It may last from 4 to 6 weeks. Use sanitary napkins—not tampons—to absorb blood or drainage.
- If you feel you need more time in hospital either because you are still not feeling confident or ready to cope with the baby on your own, please discuss this with your doctor and request to stay for a few more days. This is not an issue.
- Wound inspection is done before discharge and a new waterproof dressing is applied. Upon discharge, follow-up visit will be scheduled at day 7 or 8. You are ready to go home if you can:
# tolerate food and drinks, plus able to pass wind (flatus) without any problem.
# urinate normally
# there is progressive reduction in pain
# able to get up from bed and move around on your own
# no signs of infection
# baby can be discharged together with you (pending review by the paediatrician to give the green light that baby is fit to go home)
- Non absorbable sutures are usually removed from the skin incision on the seventh day. If absorbable suture is used, then the suture need not be removed. It will dissolve by itself after a few weeks.
- Once home, someone should be available to help care for you for the first few days.
Shower and wash your hair every as usual. Dry the incision site with dry, clean towel after each shower. - Do not douche.
- There is no specific dietary restriction. Eat a healthy and balanced diet.

- Resume daily activities and work as soon as you are able. Full recovery normally takes about 4 to 6 weeks.
- You should start postnatal exercise once you are pain-free and comfortable. Specific exercises are available for women who had a C-section. Discuss this with your nurse or doctor. Avoid heavy lifting or strenuous activity for 6 weeks.
- You can resume driving after 4 weeks, provided full mobility has returns and pain-killers medications are no longer required. Please ask your doctor if you are not sure.
- Avoid sexual intercourse for 6 weeks or as directed by your doctor.

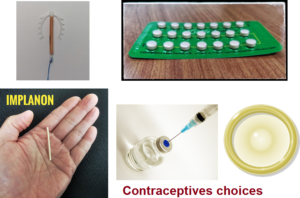
- Do not skip your postnatal visit, which is usually 6 weeks after the delivery. Discuss family planning choices with your doctor during this visit. It is advisable to avoid the next pregnancy for at least one year.
- Wound healing – a firm ridge may form along the incision. As it heals, the ridge will gradually recede. Numbness around the incision site is common. This occurs because of the cutting of the nerves when making the incision to enter the abdominal cavity. The nerves will grow back.
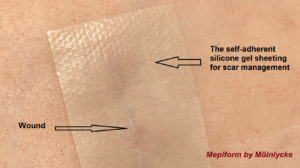
- Over time, you may also feel a mild tingling sensation and then slowly returns to normal over several months. Some women may be prone to form a thick type of scar called a keloid. If you are concern, please ask your doctor about this and your doctor may recommend some scar prevention therapy, either the gel type (apply twice a day) or a special adhesive waterproof plaster. It should be started from 7 to 14 days after Caesarean and needs to be done for at least 3-4 months to see an effect.
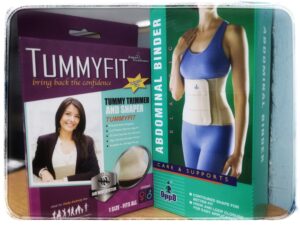
ABDOMINAL BINDER
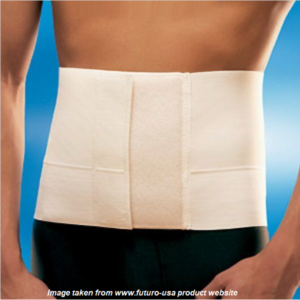 An abdominal binder is broad compression belt that encircles your abdomen. It is usually made from elastic and nylon materials with Velcro, hoop or loop closures. It comes in various shapes, sizes and softness of materials. You may want to wear one after your Caesarean section, especially if you have a pendulous abdomen (hanging belly). It may help to reduce post-operative pain and helps you to move around easily. The compression provided by the binder will also reduce the pain when you cough or sneeze. Do take note that some women do not find it useful. You should try it if you think there is a need for you. In the end, you may or may not like it.
An abdominal binder is broad compression belt that encircles your abdomen. It is usually made from elastic and nylon materials with Velcro, hoop or loop closures. It comes in various shapes, sizes and softness of materials. You may want to wear one after your Caesarean section, especially if you have a pendulous abdomen (hanging belly). It may help to reduce post-operative pain and helps you to move around easily. The compression provided by the binder will also reduce the pain when you cough or sneeze. Do take note that some women do not find it useful. You should try it if you think there is a need for you. In the end, you may or may not like it.
So far, there is no scientific evidence to proof that the use of abdominal binder (either after vaginal or caesarean delivery) will get you back in shape faster or helps you to reduce belly fat or your overall weight. It is basically used to reduce pain and provide some comfort. When choosing an abdominal binder, it is important to get the right size and wear it properly. Do make sure it is not too tight and you are able to breath and sit comfortably.
SEE YOUR DOCTOR IMMEDIATELY IF THERE IS :
- Increasing pain, swelling, redness, drainage or bleeding in the surgical area.
- Vaginal bleeding which soaks more than 1 pad or tampon each hour.
- The urge to urinate frequently, especially if associated with pain and abnormal urine colour.
- Persistent and abnormal vaginal discharge.

- Increasing nausea and vomiting.
- Short of breath or feel faint.
- Pain, swelling, and tenderness in the calf.
- You develop signs of infection, including headache, muscle aches, dizziness or a general ill feeling and fever.
- New, unexplained symptoms develop. Drugs used for treatment may produce certain side effects.
To print a pdf copy, CLICK HERE.
Please subscribe HERE to receive the regular newsletter and get the latest updates regarding Women’s Health