 We are now faced with an unprecedented pandemic due to the coronavirus. The COVID-19 is a new strain that has not been previously identified in humans. Those infected may take up to 14 days to develop symptoms. The main mode of transmission is mainly through respiratory droplets and close contacts. It may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose, or possibly their eyes, but this is not thought to be the main way the virus spreads. Routes of transmissions such as fecal-oral, in-utero from mother to baby and others are not confirmed yet. Some infected persons may be asymptomatic and they potentially can pass along the infection to others. However, this is less common. For more information about coronavirus, click here and here
We are now faced with an unprecedented pandemic due to the coronavirus. The COVID-19 is a new strain that has not been previously identified in humans. Those infected may take up to 14 days to develop symptoms. The main mode of transmission is mainly through respiratory droplets and close contacts. It may be possible that a person can get COVID-19 by touching a surface or object that has the virus on it and then touching their own mouth, nose, or possibly their eyes, but this is not thought to be the main way the virus spreads. Routes of transmissions such as fecal-oral, in-utero from mother to baby and others are not confirmed yet. Some infected persons may be asymptomatic and they potentially can pass along the infection to others. However, this is less common. For more information about coronavirus, click here and here
This article aims is to summarize and provide advice for women who are currently pregnant on the actions required in times like this. In other words, I hope this can be a simple guide to help pregnant women who need to deal with this infection during the antenatal, delivery and postnatal period. Some of the details here are specific to Malaysia, including many of the contact details and guidelines. Links will be provided for more information if you are keen to read more.
Symptoms of COVID-19 infections include fever, cough and difficulty in breathing.  In fact, it may mimic the other flu symptoms such as tiredness, body aches, runny nose, and sore throat. Some reported loose stools and loss of smell as well. Progression of symptoms will result in pneumonia in both lungs.
In fact, it may mimic the other flu symptoms such as tiredness, body aches, runny nose, and sore throat. Some reported loose stools and loss of smell as well. Progression of symptoms will result in pneumonia in both lungs.
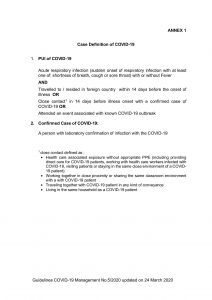
The Ministry of Health Malaysia (MOH) has published several guidelines dealing with this pandemic.
Pregnant women with confirmed COVID-19 infection should be managed by designated tertiary hospitals. The MOH Malaysia has published a list of hospitals for this purpose.
During the COVID-19 epidemic period, all pregnant women should be honest in revealing their recent travel history, any significant contact with suspected or confirmed COVID-19 cases plus any symptoms that she currently has that can be attributed to the infection.
Pregnant women may fall into any of these 4 categories:
- Currently well with no history of travel or contact with a person suspected of or confirmed COVID-19 infection. Majority of women will be in this group and pregnancy outcome will be excellent
- Recent travel from countries listed in the MOH guidelines – if you are feeling well, you need to self-quarantine for 14 days. (MOH updated this guideline (5th Edition 24th March) and removed the list of countries and specified that any traveled to / resided in a foreign country within 14 days before the onset of illness is a risk)
- Recent travel or close contacts with a confirmed case of COVID-19 AND feeling unwell (classified as a person under investigation PUI) – call the hotline and go to the nearest designated hospitals in your area. Please inform the hospital staffs that you had recent travel history or close contact. See MOH definition of PUI below
- Confirmed case of COVID-19 infections
For those in group 1, general advice will apply for prevention of infection (see section on advice during antenatal period below).
 Women in group 3 will need laboratory confirmation. COVID-19 infection can be confirmed by real-time reverse transcription polymerase chain reaction (rRT-PCR) of a specimen taken from sputum, throat swabs, lower respiratory tract secretions. The results can be obtained within the same day if sent in the morning.
Women in group 3 will need laboratory confirmation. COVID-19 infection can be confirmed by real-time reverse transcription polymerase chain reaction (rRT-PCR) of a specimen taken from sputum, throat swabs, lower respiratory tract secretions. The results can be obtained within the same day if sent in the morning.
CDC defined close contact as—
a) being within approximately 6 feet (2 meters) of a COVID-19 case for a prolonged period of time; close contact can occur while caring for, living with, visiting, or sharing a health care waiting area or room with a COVID-19 case– or –
b) having direct contact with infectious secretions of a COVID-19 case (e.g., being coughed on).
Isolation and quarantine help protect the public by preventing exposure to people who have or may have a contagious disease. CDC defined it as:
- Isolation separates sick people with a contagious disease from people who are not sick.
- Quarantine separates and restricts the movement of people who were exposed to a contagious disease to see if they become sick.
Criterias for self quarantine
- you have been in close contact with a confirmed case of COVID-19
- you recently arrived from a foreign country.
Self-quarantine should be for 14 days (see more explanation here)
- you must stay at home to prevent the possible spread of the virus to other people.
- do not go to public places such as work, school, shopping centres, childcare or university
- ask someone to get food and other necessities for you and leave them at your front door
- do not let visitors in — only people who usually live with you should be in your home
- do not need to wear a mask in your home, but do wear one if you have to go out (for example to seek medical attention)
- should stay in touch by phone and online with your family and friends
- going outside – If you live in a private house, it is safe for you to go into your garden or courtyard. If you live in an apartment or are staying in a hotel, it is also safe for you to go into the garden but you should wear a surgical mask to minimize risk to others. You should also move quickly through common areas. This helps protect yourself and others.
- monitor symptoms – if sick, do not go to your general practitioners (GP) or health clinic immediately. Please call the hotline or nearest designated hospitals.
Managing quarantine – being in guarantine for 14 days can be stressful and boring. Suggestions include:
- keep in touch with family members and friends via telephone, email or social media
- where possible, keep up normal daily routines, such as eating well and exercise
- arrange to work from home
- do things that help you relax and use isolation as an opportunity to do activities you don’t usually have time for
- advice for others living with you – if you are well, others that live with you do not need to self-isolate unless they also meet one of the isolation criteria. However, if you develop symptoms and are suspected to have COVID-19, they will be classified as close contacts and will need to be isolated.
- returning to your community – People who have completed their 14 day period without developing symptoms can return to their daily activities. To prevent the spread of viruses, practice good hygiene and social distancing.

Advise during antenatal period (when you are well and low risk)
- Practice social distancing
- Regularly wash your hand with soap and water for at least 20 seconds or use an alcohol-based hand rub if not possible. Click here for how to do it properly.
 Avoid touching your eyes, nose and mouth.
Avoid touching your eyes, nose and mouth.- Follow the routine antenatal advice, including to continue your current intake of supplements and medications prescribed by your doctor.
- Ensure that you eat a healthy and balanced diet.
- If you need to attend to your scheduled antenatal follow-up, wear a mask and follow the social distancing advice while in hospital.
- Be honest with your travel history, close contacts and any symptoms with the hospital staffs. If you are under quarantine, let your health-care provider know and stick closely to the instructions. This is for your own good and helps protect others around you.
- Admission to labour room is as per routine protocol
Infection during antenatal period
At the moment, there is no strong evidence to suggest that there is significant vertical mother to baby transmission in the third trimester. As for infection during the first or second trimester, there is not enough data or experience yet to make any conclusion. The management of the infection is similar to non-pregnant patients, with additional monitoring of fetal well-being by the obstetrics team. Following recovery, the antenatal care should not be any different but may need to get the physician involvement in follow-up as well.
Management during delivery and postnatal period in infected women or classified as PUI
If admission is required:
- women should be advised to attend via private transport where possible or call the hospital for advice as appropriate. Wear a mask. The accompanying person should also wear a mask.
- If an ambulance is required, they should be informed that the woman is currently in self-isolation for possible COVID-19.
- In the MOH guidelines, those with confirmed COVID-19 positive cases should be admitted into the designated government hospital for further management of the infection and delivery.
- For those under PUI, the women can be managed in their respective hospitals. It is important that precautions should be taken as though infection is present until laboratory confirmatory test comes back as negative.
- Women should inform the labour ward staff (by calling the hospital hotline or the labour room direct if they have the numbers) that they are coming to the hospital and asked for advice regarding the correct entrance to the labour room. Try to avoid crowded entrance if possible. The women should wait for the hospital staff and be escorted inside the delivery suite.
For those in Klang Valley, these are the designated government hospitals dealing with COVID-19.
COVID-19 infection itself is not an indication for immediate delivery unless there is an obstetric indication or a need to improve the woman’s oxygenation. The mode of delivery is still unclear, with not much evidence to guide us. At the moment, it will depend on factors such as women clinical condition, stage of labour and any other obstetrics complications. In confirmed cases of COVID-19, if the woman is already in labour and expected to be quick, then vaginal delivery can be attempted. Shortening of the second stage by either forceps or vacuum can be considered due to the fact that it is not easy to do active pushing during second stage while wearing a mask. Prolonged pushing will potentially add to the risk of further dissemination of the viral load in the room despite wearing a mask. For vaginal delivery, there are worries of prolonged exposure to staff during the entire intrapartum period and the risk of aerosol exposure is significant, especially in the second stage of labour when the patient strains or pushes. Ideally, the delivery should be conducted in a negative pressure equipped labour suite which many hospitals do not have.
In view of these factors, some guidelines recommend a Caesarean section for those suspected or Covid-19 positive women in labour¹.
For Caesarean section, both regional anesthesia and general anesthesia can be considered, depending on the clinical condition of the patient and the urgency of delivery.
For confirmed cases of COVID-19, breastfeeding is not recommended¹. Although experience in China did not show any viral particles in the breast milk of infected mothers, avoidance of breastfeeding is just precautionary advice and seems logical until we have more safety data on breastfeeding in this group of women. Routine neonatal vaccinations can be given as per protocol.  For postnatal care, the infected women and her baby may be transferred to a designated government hospital that can best manage COVID-19 cases. Those women classified as PUI should be transferred to the dedicated isolation ward for monitoring as per MOH guidelines while awaiting their laboratory confirmation of COVID-19 infection.
For postnatal care, the infected women and her baby may be transferred to a designated government hospital that can best manage COVID-19 cases. Those women classified as PUI should be transferred to the dedicated isolation ward for monitoring as per MOH guidelines while awaiting their laboratory confirmation of COVID-19 infection.
Contact:
Ministry of Health Malaysia designated hospitals for COVID-19
List of contact numbers for MOH hospitals and State Health office
Contact numbers of designated hospitals in Klang Valley and Selangor
Subang Jaya Medical Centre – Hotline 03-56391212 Labour ward 03-56391578
Article updated on 26th March 2020 – MOH guideline specified that returning from any foreign country is a risk factor
References
- MOH Guidelines Annex 23
- RCOG guidelines version 8, updated 17 April 2020
- Coronavirus infection and pregnancy – Patient information Q & A from RCOG, UK, updated 17 April 2020




 Avoid touching your eyes, nose and mouth.
Avoid touching your eyes, nose and mouth.


