The reason for practicing contraception (or birth control) is to prevent an unplanned pregnancy. Most methods of contraception enable sexually active couples to temporarily avoid pregnancy. Permanent birth control is accomplished through sterilization. There are many types of birth control methods that are currently available. There is no perfect method at the moment. Each has its own advantages and disadvantages. Be sure you know and understand the different types of birth control available to you, the risks and benefits of each, and any side effects, so that you can make an informed choice.
Combined oral contraceptives (COCs) pills prevent ovulation (release of a ripened egg from the ovary) and therefore make pregnancy unlikely. It also thickens the mucus in the cervix, making it difficult for sperm to reach an egg. The inner lining of the womb thins out during pills taking, so it is less likely to accept a fertilised egg. The combination type, combin¬ing both oestrogen and a synthetic progestogen in a fixed daily dose, are the most popu¬lar and the most effective.
Effectiveness
The effectiveness is dependant on whether the pills are taken correctly, without missing a significant number of pills. If the pills are taken according to instructions (excellent compliance), then it is almost 99 % effective. This means that less than one woman in 100 using this method for a year will get pregnant. However, in a general population, the effectiveness is slightly lower at about 91%.
Advantages
• Highly effective, with lowest failure rate of any non-permanent method—less than 0.1 pregnancies per 100 women per year, if all pills are taken as prescribed.
• Periods become more regular.
• Less painful menstrual periods (reduction in period pain)
• Decrease in the amount of menstrual bleeding in most women.
• May help with premenstrual symptoms
• Less likelihood of anaemia.
• COCs use is associated with a significant reduction in risk of endometrial and ovarian cancer that increases with duration of use and persists for many years after stopping the pills.
• Decrease in incidence of pelvic inflammatory disease.
• Use of COCs is associated with a reduced risk of colorectal cancer
• can be used for management of acne, hirsutism and menstrual irregularities associated with polycystic ovary syndrome (PCOS).
• May reduce the risk of fibroids, ovarian cysts and (non-cancerous) breast disease
Disadvantages
• Not suitable for women who are smokers and above age of 35.
• Will not protect against sexually transmitted infections (STIs). A form of barrier protection will need to be used in those at risk.
• Not suitable for those who are forgetful to take the pills on a regular basis.
• May not be suitable for some women due to side effects.
Side effects and risks
• There may be side effects from the pill. Many of these are not common and even when they do, the frequency will decrease in severity after 1 to 2 months. Most patients experience no side effects at all.
• Common mild or minor side effect may include headache, nausea, fluid retention, breast fullness or tenderness and mood changes. If these do not stop within a few months, changing the type of pill formulation or brand may help.
• Breakthrough bleeding (unexpected bleeding on pill taking days) and spotting is common in the first few months of pill use and will usually subside after a few cycles.
• Serious side effects are stroke, heart attack and blood clots in the calf veins. Fortunately, these are exceedingly rare in healthy and non-smoking women.
• Long term risks – current use of COCs for more than 5 years is associated with a small increased risk of cervical cancer; risk reduces over time after stopping COCs and is no longer increased by about 10 years after stopping. Therefore, regular cervical cancer screening via Thin Prep is important. Recently, there is data to suggest that there is slight increase in breast cancer risk in long term users. However, the net increase is still exceedingly small and not a concern if you have gone through a thorough clinical examination and no contra-indication to start the pills. It is also reassuring to note that there is a large epidemiological data to suggest an overall net reduction of all types of cancer in pill users as well.
Instructions – When and How to start?
There are many conditions that might make the pill unsuitable for you. Your doctor will take a thorough medical history and perform a physical examination prior to prescribing combined oral contraceptives. If any of the conditions are present that makes the pills unsuitable, another form of birth control will be recommended.
When?
• During menses – starts from day 1 onwards but not later than day 5. You will be protected from pregnancy immediately.
• Starts immediately upon switching from other methods such as injectables type, implants or intrauterine device. You will be protected from pregnancy immediately.
• Can start from 6 weeks onwards following delivery if you are not breastfeeding. If you are still breast feeding, please discuss with your doctor and you may want to consider other options
• Immediately after miscarriage or ectopic pregnancy
How?
To start the first pack:
• Count the first sign of your menstrual bleeding as day 1. On either day 1, 2 or 3, begin taking 1 pill each day. Pick a time that suits you and stick to it as your routine. The effect of pregnancy prevention by the pills is immediate. However, if you start the pill only after the 5th day, additional contraceptive protection (e.g using condoms) is required for 7 days before the pills is able to offer the pregnancy prevention effect.
• For those who start following delivery, miscarriage, ectopic pregnancy or changing from another method, first day of pill taking will be Day 1
• You can start anytime in your menstrual cycle, provided you are sure you are not pregnant or there was no prior unprotected sex.
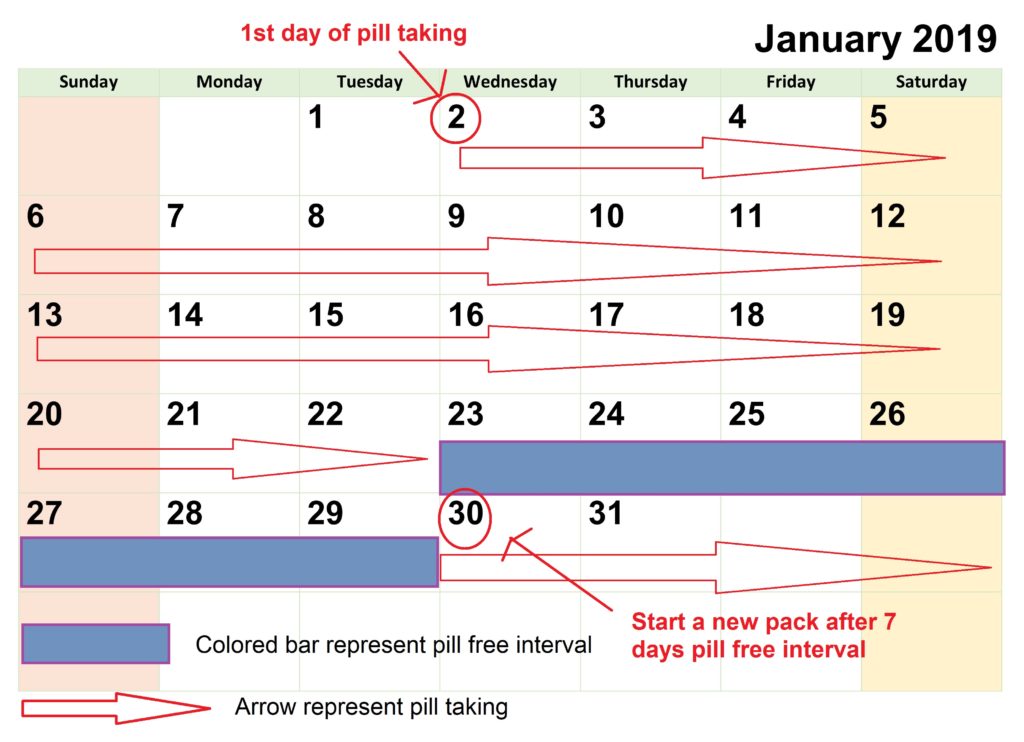
• Continue taking the pills for 21 days. Use a method to remind you daily to take the pill. Set up an alarm daily in your mobile device and swallow the pill immediately when the alarm goes off. Fluid is not necessary, and you can swallow it with saliva to ensure that you do not forget.
• Stop taking the pills for 7 days once you finish the 21 days pack (this is called the pill free interval).
• Begin taking pills again for the next cycle after these 7 days of rest, no matter when menstrual bleeding begins or ends. You should still start even though you are still menstruating on the day you are supposed to start a new pack.
• If you do not have menses during the pill free interval, do not start the next pack. See your doctor first for further evaluation. This can occur in a small minority of women and can be normal. However, pregnancy needs to be excluded first.
• If for whatever reasons you want to delay your period, you can continue to the next pack without stopping (no pill free interval). There will be no bleeding as long as the pills are taken. You can take 2 or 3 packs continuously without a break. There are no additional risks.
• If you forget to take the pill/pills, please refer to the patient information leaflet on missed COCs pills.
Calendar showing example of 21 days pills taking and the 7 days pill free internal
Factors that affect effectiveness of COCs
• Effectiveness may be reduced in women who have had bariatric surgery
• Women using enzyme-inducing drugs
Most broad-spectrum antibiotics are does not affect COCs and no additional contraceptive precaution is required unless the antibiotics (and/or illness) cause vomiting or severe diarrhoea. If vomiting occurs within 3 hours of taking COCs, take another pill. If severe diarrhoea occurs for >24 hours, you should consider this as missed pills. Refer to pamphlet on missed pills for advice.
See your doctor immediately if there is:
• Increased frequency, amount, or duration of menstrual bleeding.
• Painful during intercourse or bleeding afterward.
• Pain and swelling in the calf of your leg, or any unusual leg pains.
• Severe chest pain or shortness of breath.
• Blood pressure goes up.
• Symptoms of gallbladder disease: upper abdominal pain, fever, jaundice, nausea.
• Any signs or symptoms that make you suspect pregnancy.
• See flashing lights or blurred images, or your ability to see decreases.
• Severe, throbbing headache.
Download this article in pdf here.
[mailerlite_form form_id=3]